
As a specialized pain management practice, we frequently treat patients with sacral fractures. A sacral fracture is a break in the sacrum, the triangular bone at the base of the spine. These fractures can cause significant pain and mobility issues, affecting daily life. The pain can be severe, often making it difficult to sit, stand, or walk comfortably. Finding a position of relief can be challenging, as movement frequently exacerbates discomfort. In some cases, nerve involvement can lead to additional symptoms such as numbness or tingling in the legs.
Where Do You Feel Pain From a Sacral Fracture?
Pain from a sacral fracture is typically felt in the lower back, buttocks, and hips. Unlike general lower back pain from muscle strain or arthritis, sacral fracture pain is often deep, persistent, and worsens with weight-bearing activities. It may not improve with traditional treatments like stretching or heat therapy. Patients often report sharp, localized pain that radiates into the pelvis or legs, making standing, sitting, or walking particularly difficult. Many patients also experience pain radiating into the pelvis or upper thighs. Depending on the severity, nerve involvement may lead to numbness, tingling, or weakness in the legs. Sitting or standing for long periods often worsens symptoms. Some patients report sharp, stabbing pain, while others experience a dull, persistent ache. Pain can also intensify with movements such as transitioning from sitting to standing, bending forward, or even slight shifts in body weight. In more severe cases, sacral fractures may affect bladder and bowel function, requiring urgent medical evaluation. The discomfort often leads to difficulty sleeping, affecting overall quality of life. Early recognition of these symptoms is crucial for effective management and timely treatment.
How Do Sacral Fractures Happen?
Sacral fractures occur due to:
- Trauma: Falls, car accidents, or high-impact injuries can break the sacrum. These injuries often occur during direct impacts to the lower back or pelvis, such as in sports-related collisions or severe slips and falls. In elderly individuals, even a minor fall can result in a sacral fracture due to age-related bone weakening. High-energy trauma, like motor vehicle accidents, can lead to more complex fractures, sometimes involving nerve damage and severe pain.
- Osteoporosis: Weakened bones from osteoporosis increase the risk of stress fractures, even from minor falls or normal daily activities. Over time, reduced bone density makes the sacrum more vulnerable to fractures, even during routine movements like bending, lifting, or rising from a chair. Many individuals with osteoporosis-related sacral fractures may experience chronic pain before diagnosis, often mistaking it for general lower back discomfort. Since osteoporosis is often a silent disease, these fractures can serve as the first noticeable sign of weakened bones, emphasizing the importance of bone health management and early intervention.
- Cancer: Bone metastases from cancers like breast, lung, prostate, and multiple myeloma can weaken the sacrum and cause pathological fractures. These fractures occur when cancerous cells spread to the bone, disrupting normal bone remodeling and making the sacrum more susceptible to fractures even with minimal stress. Patients with cancer-related sacral fractures often experience worsening pain that is not relieved by rest and may be accompanied by other symptoms such as unexplained weight loss or fatigue. In some cases, these fractures can be the first sign that cancer has metastasized, making early detection and intervention critical.
- Repetitive stress: High-impact activities such as long-distance running or military training can lead to stress fractures over time.
Osteoporosis and Sacral Fractures
Osteoporosis is a major risk factor for sacral fractures. As bones lose density, they become brittle and more likely to break under normal pressure. These fractures can develop insidiously, often without a clear traumatic event. Many patients with osteoporosis-related sacral fractures don’t recall a specific injury, as these breaks can occur from routine activities like standing up too quickly, minor falls, or even prolonged periods of sitting or bending. Over time, microfractures can accumulate, leading to structural weakness and an increased risk of more severe fractures. Identifying osteoporosis early and implementing bone-strengthening strategies, such as weight-bearing exercises and calcium and vitamin D supplementation, can play a crucial role in prevention.
Cancer and Sacral Fractures
Cancer that spreads to the bones, especially from prostate, breast, lung, or multiple myeloma, can cause sacral fractures. These fractures often occur because cancer disrupts normal bone remodeling, leading to structural weakness. When cancer weakens the sacrum, even minimal stress, such as walking or standing, can result in a break. Patients with cancer-related sacral fractures may experience persistent, deep-seated pain that does not improve with rest and worsens over time. Additional symptoms such as swelling, reduced mobility, and neurological complications, including numbness or weakness in the lower extremities, may also be present. Identifying cancer-related fractures early is crucial because treatment focuses not only on pain relief but also on managing the underlying disease to prevent further skeletal complications.
Treatment Options for Sacral Fractures
Treatment depends on the cause and severity of the fracture.
Conservative Management
- Rest & Activity Modification: Limiting weight-bearing activities reduces stress on the sacrum. In most cases, patients are advised to avoid full weight-bearing on the affected side for several weeks, typically using crutches or a walker for support. Non-weight-bearing or partial weight-bearing status is often recommended depending on the severity of the fracture, and physicians may adjust these restrictions as healing progresses. Gradual reintroduction of weight-bearing activities under medical supervision ensures a safer recovery.
- Pain Management: Over-the-counter or prescription pain medications help control symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can reduce inflammation and provide relief, while acetaminophen can help manage pain without causing stomach irritation. In cases of severe pain, physicians may prescribe short-term use of stronger medications like opioids. Additionally, nerve pain medications such as gabapentin or duloxetine may be beneficial if nerve involvement is present. Adjunctive therapies like heat and ice application, topical analgesics, and relaxation techniques can further aid in pain relief.
- Bracing: A sacral orthotic brace can provide stability and reduce discomfort.
- Physical Therapy: Strengthening surrounding muscles improves mobility and reduces strain on the sacrum. Physical therapy typically begins 4 to 6 weeks after the initial diagnosis, once the fracture has shown signs of healing and pain levels have decreased. The program is tailored to gradually restore strength, flexibility, and balance while minimizing the risk of reinjury.
Bone Tumor Ablation for Sacral Fractures
For patients with tumor-related sacral fractures, bone tumor ablation can be an effective option to reduce pain. This procedure involves using thermal energy to target and destroy cancerous bone lesions before stabilizing the fracture. By reducing the tumor burden, bone tumor ablation can provide significant pain relief and improve mobility, often in combination with sacroplasty.
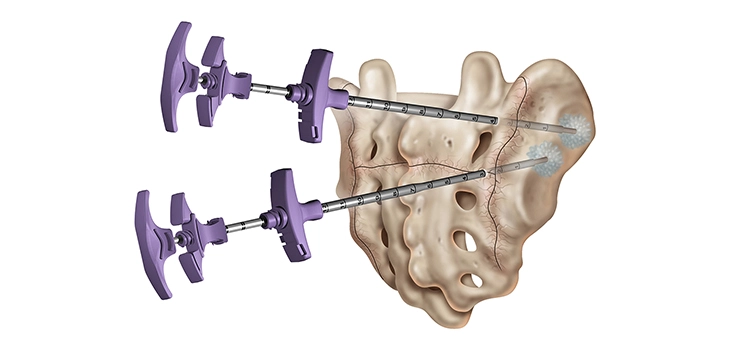
Sacroplasty: A Minimally Invasive Option
For patients with persistent pain or fractures that fail to heal, sacroplasty offers a minimally invasive treatment option. This procedure involves injecting medical-grade cement into the fractured sacrum to stabilize the bone and reduce pain. Most patients experience immediate pain relief and improved mobility.
Benefits of Sacroplasty
- Rapid Pain Relief: Many patients report significant pain reduction within 24 hours of the procedure.
- Minimally Invasive: The procedure requires only a small incision, reducing recovery time and risk of complications.
- Improved Mobility: By stabilizing the sacrum, sacroplasty helps restore function and allows patients to regain independence.
- Reduced Need for Pain Medication: Patients often decrease or discontinue their reliance on pain medications post-procedure.
Risks of Sacroplasty
- Cement Leakage: Although rare, small amounts of cement may leak outside the bone, potentially irritating surrounding tissues.
- Infection: Any procedure carries a small risk of infection, though this is minimized with sterile techniques.
- Nerve Irritation: Some patients experience temporary nerve pain after the procedure, which usually resolves quickly.
Success Rates
Sacroplasty has shown high success rates, with studies indicating pain relief in over 85% of patients. According to a study published in the Journal of Pain Research, sacroplasty provides long-term pain relief and functional improvement, particularly for patients with osteoporotic fractures. Long-term outcomes suggest improved quality of life and functional recovery, particularly for those with osteoporosis-related fractures. While results may vary, sacroplasty remains one of the most effective treatments for sacral fractures, particularly when conservative management fails.
How Sacroplasty Compares to Kyphoplasty and Vertebroplasty
Sacroplasty is similar to kyphoplasty and vertebroplasty, two procedures used to treat vertebral compression fractures. Here’s how they compare:
| Procedure | Bone Treated | Balloon Used? | Goal |
|---|---|---|---|
| Sacroplasty | Sacrum | No | Stabilize the sacral fracture |
| Vertebroplasty | Spine (vertebrae) | No | Stabilize a vertebral fracture |
| Kyphoplasty | Spine (vertebrae) | Yes | Restore height and stabilize the fracture |
- Sacroplasty and vertebroplasty both involve cement injection without height restoration.
- Kyphoplasty differs by using a balloon to restore vertebral height before injecting cement.
When to Seek Treatment
If you experience persistent lower back or pelvic pain, especially after a fall or if you have osteoporosis or cancer, seek medical attention as soon as possible. Early diagnosis of a sacral fracture can prevent complications and lead to faster recovery. Delayed treatment may result in worsening pain, reduced mobility, and potential nerve involvement. Over time, untreated sacral fractures can lead to chronic pain, postural changes, and increased risk of additional fractures due to altered weight distribution. In severe cases, prolonged instability in the sacrum may contribute to spinal misalignment, making movement increasingly difficult and reducing overall quality of life. Diagnostic imaging, including X-rays, CT scans, or MRI, can confirm the fracture and guide the best treatment approach. Seeking timely medical care ensures proper management and improves the chances of a successful recovery.
Conclusion
Sacral fractures can cause severe pain and disability but are treatable with conservative care or sacroplasty. Understanding the risk factors, especially osteoporosis and cancer, can help with early detection and proper management. If you suspect a sacral fracture, contact a specialist to discuss your options.
Schedule an Appointment
At Red Butte Pain Solutions, we offer advanced treatments for sacral fractures, including sacroplasty. Call us at 602-633-4334 or schedule an appointment today.
