Head, Neck & Facial Pain
Cervical Facet Arthropathy
Related Topics:

Neck pain is a common complaint that can significantly impact daily life. One frequent cause of chronic neck discomfort is cervical facet arthritis, also known as cervical facet arthropathy. This condition arises from degenerative changes in the small joints of the neck, called facet joints. These joints play a vital role in neck movement, and when they become inflamed or damaged, they can lead to pain and stiffness.
What is Cervical Facet Arthropathy?
Cervical facet arthropathy refers to arthritis or degeneration in the facet joints of the cervical spine (neck). These joints provide stability while allowing the neck to bend and rotate. Over time, wear and tear, poor posture, or trauma can lead to joint inflammation, cartilage loss, and pain.
Symptoms of Cervical Facet Arthropathy
- Localized neck pain that worsens with movement
- Stiffness or reduced range of motion in the neck
- Pain that radiates to the shoulders or upper back
- Headaches, often at the base of the skull
Cervical Facet Referral Patterns
The cervical spine consists of seven vertebrae labeled C1 through C7. These vertebrae are divided into three regions:
- Upper neck: Includes C1 (atlas) and C2 (axis), which provide rotation and support for the skull.
- Mid-neck: Includes C3 through C5, where most neck bending and extension occur.
- Lower neck: Includes C6 and C7, connecting the cervical spine to the thoracic spine and shoulders.
Facet joints are located at the back of each vertebra, linking one vertebra to the next. These joints allow smooth neck movements and provide stability. When they become arthritic, they can refer pain to various areas depending on the level of the affected joint.

Common Cervical Facet Referral Patterns:
- C2-C3 joints: Pain referred to the base of the skull or behind the eyes.
- C3-C4 joints: Pain radiating to the back of the neck and shoulders.
- C5-C6 joints: Pain spreading to the shoulder blades and upper arms.
Understanding these referral patterns is crucial for accurately diagnosing and targeting the source of pain.
Neck Pain and Headaches
Cervical facet arthritis is a significant cause of neck pain and headaches, particularly cervicogenic headaches. These headaches originate in the cervical spine but are often felt in the head, leading to confusion with migraines or tension headaches.
How Cervical Facet Arthropathy Causes Headaches:
- Upper cervical joints, such as C2-C3, are closely linked to headache symptoms due to their connection to the brainstem and surrounding nerves.
- The third occipital nerve, which originates from the C3 nerve root, is particularly important. Irritation of this nerve, often from arthritis in the C2-C3 joint, can lead to pain radiating to the back of the head, temples, or even behind the eyes.
- Chronic inflammation or instability in the upper cervical facet joints can trigger tension in surrounding muscles, worsening headache symptoms.
Patients often find relief when their neck pain is addressed, demonstrating the close relationship between neck conditions and headaches.
Causes of Cervical Facet Arthritis
Several factors contribute to the development of cervical facet arthritis, including age, lifestyle habits, and previous injuries.
Age-Related Degeneration
The most common cause of cervical facet arthritis is natural wear and tear. Over time, the cartilage within the facet joints breaks down, leading to inflammation, stiffness, and pain.
Poor Posture and “Text Neck”

Modern lifestyles often involve prolonged use of smartphones and computers, leading to a condition called text neck. This posture, characterized by a forward head tilt, places excessive strain on the facet joints and accelerates their degeneration. Addressing posture can significantly reduce the risk of developing facet arthritis.
Whiplash Injuries
Whiplash, often caused by car accidents, is another significant contributor to cervical facet arthritis. During a whiplash injury:
- The neck undergoes rapid extension and flexion, causing damage to the facet joints.
- This trauma can lead to microtears in joint ligaments, resulting in long-term instability.
- Over time, repeated strain from an unstable joint can cause arthritis, leading to chronic pain.

Conservative Treatment Options for Cervical Facet Arthropathy
Managing cervical facet arthritis often begins with conservative treatments. These approaches aim to reduce pain, improve mobility, and prevent further joint degeneration.
Medications
- NSAIDs (e.g., ibuprofen or naproxen): Reduce pain and inflammation.
- Muscle relaxants: Alleviate muscle spasms that often accompany facet arthritis.
- Topical analgesics: Provide targeted pain relief without systemic side effects.
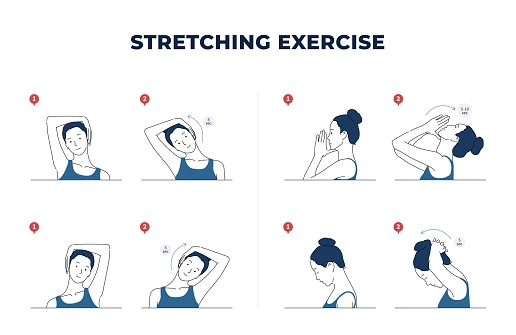
Physical Therapy
- Posture correction: Helps alleviate stress on the facet joints.
- Strengthening exercises: Builds support for the neck to reduce strain on the joints.
- Stretching routines: Improves flexibility and range of motion.
Heat and Cold Therapy
- Ice packs: Reduce swelling during acute pain episodes.
- Heating pads: Relax tight muscles and improve blood flow to the area.
Injections
Cervical facet joint injections can provide temporary relief by delivering anti-inflammatory medication directly to the source of pain. These injections can also help confirm the diagnosis.
Radiofrequency Ablation for Cervical Facet Arthritis
When conservative treatments don’t provide lasting relief, radiofrequency ablation (RFA) offers a minimally invasive option. This procedure interrupts pain signals from the affected facet joints, providing longer-lasting relief compared to injections.
How Neck Ablation Works:
- A specialist identifies the affected nerves using imaging guidance.
- A small needle delivers radiofrequency energy to disrupt the nerve’s ability to transmit pain.
- Relief typically lasts between 6 and 18 months, with some patients experiencing even longer benefits.
RFA is particularly effective for patients with chronic pain or recurring headaches caused by cervical facet arthritis.
When to Seek Treatment
If neck pain persists despite conservative measures, it’s time to consult a specialist. Timely treatment can prevent worsening symptoms and improve your quality of life. At Red Butte Pain Solutions, we offer personalized care for conditions like cervical facet arthritis, combining evidence-based therapies with advanced procedures to achieve lasting relief.
Regain Control Over Neck Pain
Living with cervical facet arthropathy can be challenging, but effective treatments are available. Understanding the condition’s causes, referral patterns, and connection to neck pain and headaches can empower you to take the next steps toward relief. Whether it’s improving posture, finding the right pillow, or considering advanced treatments like neck ablation, there’s a solution for every patient.
If you’re ready to tackle your neck pain, call Red Butte Pain Solutions today at 602-633-4334. Our team is dedicated to providing a tailored approach to help you get back to doing what you love.
Back of Head and Neck Pain: Causes and Relief Options
Pain in the back of the head and neck can be frustrating, exhausting, and surprisingly complex. Two common causes of this pain are occipital neuralgia and cervicogenic headaches. While they affect the same general region, they differ in their origins, symptoms, and...
Left Arm Pain: Heart Attack or Cervical Radiculopathy?
Left arm pain is often a cause for concern, as many people immediately associate it with a heart attack. However, other conditions, such as cervical radiculopathy, can also cause similar discomfort. Understanding the differences between these conditions is essential...
Neck Pain Symptoms and Cancer: When To Be Concerned?
Neck pain is a common complaint, often caused by muscle strain, arthritis, or poor posture. However, certain neck pain symptoms may indicate cancer, requiring timely evaluation and care.com/pain/head-neck-facial-pain/#facet-arthritis), or poor posture. However, in...
Radiofrequency Ablation: Relief for Chronic Pain
At Red Butte Pain Solutions, radiofrequency ablation (RFA) is one of our most effective tools for treating chronic pain. This minimally invasive procedure uses heat generated by radio waves to target specific nerves and disrupt their ability to transmit pain signals....
Deep Dive: Transforaminal Epidural Steroid Injection
One of the most frequent injections I perform is a transforaminal epidural steroid injection. I'm often asked by patients, particularly women, "Is this like an epidural when you have a baby?" And I get to explain that it's really something altogether different. If...
Epidural Steroid Injections: Isn’t This Just a Band-Aid?
Epidural steroid injections are one of the most common procedures I perform. This is in no small part due to the fact that every year one of the top reasons people see a doctor is back pain. Patients often have questions like, “How does the steroid work to stop the...
Let’s Talk About Your Neck and Headache Pain…
Cervicogenic headaches are a common but often misunderstood condition that connects neck and headache pain. If you’ve experienced persistent headaches accompanied by neck discomfort, cervicogenic headaches might be the cause. Understanding their symptoms, causes, and...
Neck Pain and Headaches: Diagnosing and Treating Them
Neck pain can significantly affect your daily activities, especially when it leads to cervicogenic headaches. These headaches originate in the neck and can spread to the head, causing discomfort and reduced function. A friend of mine, a jewelry maker, experiences neck...
Waking Up to Neck Pain
This morning, like many others, you might have woken up to a stiff neck that limits your movement and causes discomfort throughout the day. At Red Butte Pain Solutions, we understand the impact of neck pain on daily life, especially when it's caused by conditions like...
Overcoming Neck Pain
Lots of people have Neck pain. It can happen because of things like getting hurt, sitting or standing the wrong way, feeling stressed, getting older, or having arthritis. Neck pain can be a little bit painful or very painful. It can make it hard to do everyday things...
Cervical Radiculopathy
Related Topics:
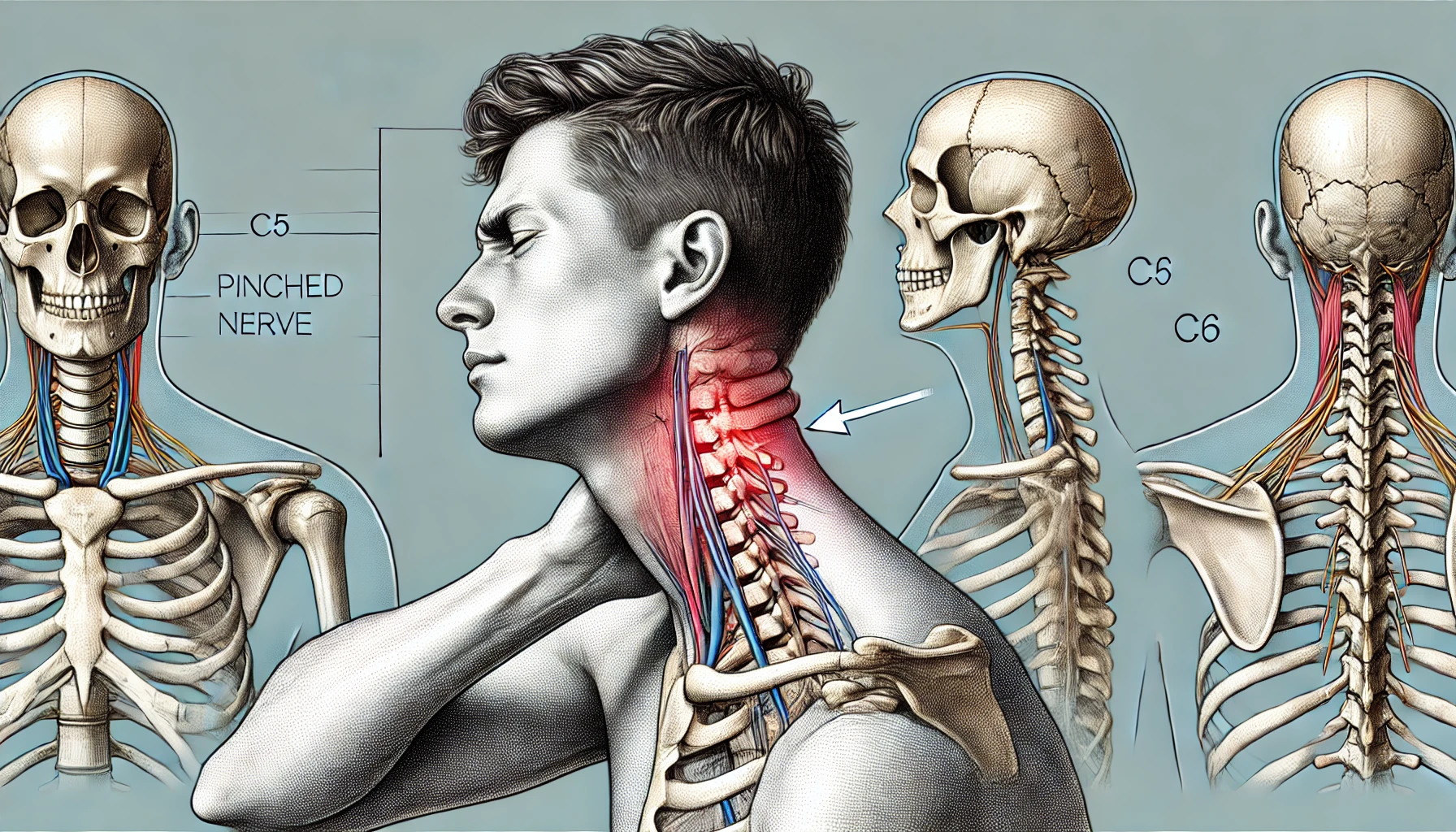
Cervical radiculopathy, often referred to as a pinched nerve in the neck, occurs when a nerve root in the cervical spine becomes compressed or irritated. This condition can cause pain, weakness, numbness, or tingling that radiates into the shoulders, arms, and hands. Whether caused by aging, injury, or lifestyle factors, cervical radiculopathy can disrupt daily life.
This guide covers the causes, symptoms, diagnosis, and treatment options for cervical radiculopathy, providing the information you need to understand and manage this condition effectively.
What is Cervical Radiculopathy?
The cervical spine comprises seven vertebrae (C1 to C7), which provide structure, mobility, and protection for the spinal cord. Between these vertebrae are spinal discs that cushion and absorb shock during movement. Emerging from each level of the cervical spine are nerve roots, which transmit signals between the brain and specific areas of the body, such as the shoulders, arms, and hands.
Cervical radiculopathy occurs when one or more of these nerve roots are compressed or inflamed, leading to symptoms along the nerve’s pathway. This compression often results from degenerative changes in the spine, injury, or other conditions that alter the spinal structure.
Symptoms of Cervical Radiculopathy
Cervical radiculopathy can present with a variety of symptoms depending on the specific nerve root affected. Common symptoms include:
- Radiating Pain: Pain often begins in the neck and radiates into the shoulder, arm, or hand.
- Weakness: Some individuals experience weakness in their arm or hand, making it difficult to perform tasks requiring grip or fine motor skills.
- Tingling or Numbness: A pins-and-needles sensation or loss of feeling is common, especially in the fingers.
- Reflex Changes: Reflexes in the affected limb may become diminished.
For instance, if the C6 nerve root is affected, the pain may radiate to the thumb, accompanied by weakness in the biceps. In contrast, compression of the C7 nerve root might cause discomfort in the middle finger and weakness in the triceps.

Symptom Locations by Affected Nerve Roots:
- C5: Shoulder pain and weakness in the deltoid muscle.
- C6: Pain radiating to the thumb, with bicep weakness and reduced bicep reflex.
- C7: Pain radiating to the middle finger, tricep weakness, and reduced tricep reflex.
- C8: Pain in the pinky and ring fingers, with weakness in grip strength.
What Causes Cervical Radiculopathy?
Degenerative Disc Disease and Herniation
Age-related changes in the cervical spine are a leading cause of cervical radiculopathy. Over time, spinal discs lose water content and flexibility, making them more prone to bulging or herniation. When a disc herniates, its inner material can press against nearby nerve roots, causing pain and irritation.
Bone Spurs
As part of the aging process or in response to arthritis, the body may develop bony growths called osteophytes or bone spurs. These can encroach on the space available for nerves, leading to compression.
Spinal Stenosis
Spinal stenosis refers to the narrowing of the spinal canal or foramina (the openings through which nerves exit the spine). This narrowing can compress nerve roots, particularly in older adults.
Trauma and Repetitive Strain
Injuries from car accidents, sports, or falls can damage the cervical spine. Whiplash injuries, for example, can strain or destabilize the neck’s structures, leading to radiculopathy over time. Repetitive motions, such as prolonged overhead work, can also contribute to nerve irritation.
Other Causes
Less commonly, tumors, infections, or systemic conditions like rheumatoid arthritis can compress cervical nerve roots.
Diagnosing Cervical Radiculopathy
An accurate diagnosis of cervical radiculopathy is essential for effective treatment. The process typically begins with a detailed medical history and physical examination.
Medical History and Physical Examination
During the evaluation, your healthcare provider will ask about the onset, location, and severity of your symptoms. They may also assess muscle strength, reflexes, and sensation in the affected areas to identify the specific nerve root involved.
Imaging Studies
Imaging plays a crucial role in confirming the diagnosis.
- MRI scans provide detailed images of soft tissues, including discs and nerves, and are often the first-choice imaging method.
- X-rays can identify bone spurs, fractures, or misalignment in the cervical spine.
- CT scans, sometimes combined with myelography, offer additional detail on bony structures and nerve root compression.
Electrodiagnostic Testing
If the diagnosis remains unclear, tests such as electromyography (EMG) or nerve conduction studies may be performed to evaluate the function of the affected nerve and rule out other conditions like peripheral neuropathy or carpal tunnel syndrome.
Treatment Options for Cervical Radiculopathy
Treatment for cervical radiculopathy focuses on relieving symptoms, improving function, and addressing the underlying cause. Most patients respond well to non-surgical methods, but surgery may be necessary in severe cases.
Non-Surgical Treatments
Conservative treatments are the first-line approach and often involve a combination of therapies:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can reduce inflammation and pain. In some cases, muscle relaxants or nerve-pain medications like gabapentin may be prescribed.
- Physical Therapy: A tailored physical therapy program can strengthen neck and shoulder muscles, improve posture, and reduce nerve root compression. Therapists may also use traction to gently stretch the spine and create more space for the nerve.
- Activity Modification: Patients are advised to avoid activities that exacerbate symptoms, such as heavy lifting or prolonged computer use. Ergonomic adjustments at workstations can also alleviate strain on the cervical spine.
- Epidural Steroid Injections: For more severe symptoms, epidural steroid injections near the affected nerve root can provide effective pain relief.
Surgical Options
Surgery is considered when conservative treatments fail to provide relief or when symptoms worsen, such as significant weakness, persistent pain, or loss of function. Common surgical procedures for cervical radiculopathy include:
- Laminectomy: This procedure involves removing part of the vertebra’s bony arch (lamina) to create more space in the spinal canal. A laminectomy is often performed in cases of spinal stenosis or significant nerve compression.
- Foraminotomy: In this procedure, the surgeon enlarges the foramina (openings through which nerves exit the spine) to relieve pressure on the affected nerve. This is particularly effective for cases of foraminal stenosis caused by bone spurs or disc degeneration.
- Anterior Cervical Discectomy and Fusion (ACDF): ACDF is one of the most commonly performed procedures for cervical radiculopathy caused by herniated discs or severe degenerative changes. During this surgery:
- The surgeon removes the problematic disc or bone spur through a small incision in the front of the neck.
- The space between the vertebrae is filled with a bone graft or synthetic spacer to maintain height and alignment.
- A plate and screws are often used to stabilize the spine while the graft fuses with the surrounding vertebrae.
ACDF not only decompresses the nerve but also stabilizes the affected spinal segment, preventing future issues at that level. While it limits motion at the fused segment, most patients maintain excellent overall neck mobility.
ACDF has a high success rate and is particularly effective at relieving nerve-related symptoms like radiating pain and weakness. Recovery typically involves a short hospital stay and several weeks of physical therapy to restore strength and flexibility.
Living with Cervical Radiculopathy: Lifestyle Modifications
Adopting healthy habits can help prevent cervical radiculopathy or reduce the likelihood of recurrence. Maintaining good posture, incorporating neck-strengthening exercises, and using ergonomic tools at work are essential. Additionally, maintaining a healthy weight and staying active can reduce stress on the cervical spine.

Conclusion
Cervical radiculopathy can cause significant pain and discomfort, but effective treatments are available. Understanding the condition’s causes, symptoms, and available therapies empowers individuals to seek timely care and make informed decisions about their health.
If you’re experiencing persistent neck pain or suspect cervical radiculopathy, contact Red Butte Pain Solutions today at 602-633-4334. Our team specializes in diagnosing and treating conditions of the cervical spine, offering personalized care to help you regain your quality of life.
Facial Pain / Trigeminal Neuralgia
Related Topics:
Understanding Trigeminal Neuralgia
Trigeminal neuralgia is a chronic condition that causes sudden, intense pain episodes, typically on one side of your face. This pain can disrupt your daily activities and significantly impact your quality of life. At Red Butte Pain Solutions, we’re committed to helping you understand this condition and explore the treatment options available.
What Causes Trigeminal Neuralgia?
Trigeminal neuralgia occurs when the trigeminal nerve’s function is disrupted. This nerve carries sensation from your face to your brain. The disruption can be due to:
- Contact between a blood vessel and the trigeminal nerve at the base of the brain.
- Damage to the myelin sheath, the protective coating around nerves.
- A tumor compressing the trigeminal nerve.
- Ageing or brain injury.
Symptoms of Trigeminal Neuralgia
The primary symptom of trigeminal neuralgia is severe shooting pain that may feel like an electric shock. Other symptoms include:
- Pain triggered by touching the face, biting, talking, or brushing.
- Pain areas include the ear, eyes, forehead, jaw, mouth, and face.
- Over sensitivity, sensitivity to pain, or uncomfortable tingling and burning.
Management and Treatment Options
Treatment for trigeminal neuralgia includes medication and surgery. Medications such as anticonvulsants and anti-spasmodic drugs can help manage the pain. In some cases, surgical procedures may be necessary.
One such procedure is trigeminal nerve ablation. We invite you to learn more about this treatment option on our website.
Serving Arizona Communities
At Red Butte Pain Solutions, we’re dedicated to serving patients with facial pain in Chandler, Tempe, Ahwatukee, Phoenix, Sun Lakes, Maricopa, Casa Grande, Mesa, Gilbert, and Laveen, Arizona. Our team of experts is here to help you navigate your pain management journey.
Remember, you don’t have to live with the pain. Reach out to us today for a consultation.
Understanding Facial Pain and Trigeminal Neuralgia
Facial pain can be one of the most distressing and intense types of pain a person can experience. In 2020, I faced this firsthand when a tooth infection spread into my face, causing unbearable pain. The infection led to emergency surgery, and even with just a 50%...
Occipital Neuralgia
Related Topics:

Do you experience sharp, shooting pain starting at the base of your skull? Does it radiate across your scalp or even behind your eyes? This type of discomfort can be intense and life-disrupting. If this sounds familiar, you may be dealing with occipital neuralgia. Let’s explore this condition, what causes it, and how it can be treated to improve your quality of life.
What Is Occipital Neuralgia?
Occipital neuralgia is a chronic pain condition that affects the occipital nerves. These nerves originate in the upper spine and travel through the scalp, providing sensation to the back of your head. When these nerves become irritated, compressed, or damaged, they can trigger sharp, electric-like pain.
Occipital neuralgia is often confused with migraines or tension headaches, but it’s a separate condition with its own causes and treatments. Accurate diagnosis is key to finding relief.
What Causes Occipital Neuralgia?
Several factors can lead to occipital neuralgia, but the underlying issue is usually irritation or injury to the occipital nerves. Common causes include:
-
- Nerve Compression: Tight muscles in the neck or scalp can put pressure on the nerves.
- Injury or Trauma: A head or neck injury, even a minor one, may damage the nerves.
- Arthritis: Degeneration in the cervical spine can irritate the nerve roots.
- Postural Strain: Poor posture or repetitive neck movements can lead to chronic tension in the area.
- Underlying Health Conditions: Diabetes, infections, or even tumors can affect nerve function.
Identifying the root cause is essential for choosing the best treatment.
Recognizing the Symptoms of Occipital Neuralgia
Occipital neuralgia has distinct symptoms that help differentiate it from other types of headaches:
-
- Sharp, Stabbing Pain: The pain often starts at the base of the skull and radiates upward.
- Tenderness in the Scalp: Even gentle touch can cause discomfort.
- Pain Behind the Eyes: This symptom is common and can feel like pressure or throbbing.
- Unilateral or Bilateral Pain: Pain can affect one or both sides of the head.
- Neck Pain or Stiffness: This often accompanies the headache, creating a sensation of tightness.
If these symptoms resonate with you, consult a healthcare provider to discuss your options.
How Is Occipital Neuralgia Diagnosed?
Diagnosing occipital neuralgia involves a detailed medical history and physical exam. A healthcare provider may press on specific areas around the occipital nerves to see if the pain is triggered. Additional tests, such as imaging studies (MRI or CT scans), may be used to rule out other conditions.
A diagnostic nerve block—an injection of a local anesthetic near the occipital nerves—can confirm the diagnosis. If the block relieves your pain, it’s likely that the occipital nerves are the source of the problem.
How Is Occipital Neuralgia Treated?
There’s no one-size-fits-all approach to treating occipital neuralgia, but there are several effective options. Treatment often begins with conservative methods and progresses to more advanced interventions if needed.
-
- Conservative Treatments
- Heat or Ice Therapy: Applying heat can relax muscles, while ice reduces inflammation.
- Massage Therapy: Gently massaging the neck and scalp can ease tension and improve circulation.
- Stretching Exercises: Neck stretches can improve posture and reduce muscle tightness.
- Lifestyle Adjustments: Ergonomic workspaces and regular breaks from screen time can help prevent flare-ups.
- Medications
- Over-the-Counter Pain Relievers: NSAIDs like ibuprofen can help reduce inflammation and mild pain.
- Prescription Medications: Drugs like gabapentin or pregabalin target nerve-related pain effectively.
- Muscle Relaxants: These can relieve spasms that compress the occipital nerves.
- Interventional Procedures
- If conservative methods aren’t enough, your provider might recommend:
- Nerve Blocks: Injections of anesthetics and steroids provide temporary pain relief and reduce inflammation.
- Botox Injections: These relax muscles around the occipital nerves, reducing compression and irritation.
- Radiofrequency Ablation (RFA): This minimally invasive procedure uses heat to interrupt pain signals from the affected nerves.
- Surgical Options
- For severe, unrelenting cases, surgical interventions may be considered:
- Occipital Nerve Decompression: Removes pressure from the nerves by addressing surrounding tissues.
- Peripheral Nerve Stimulation: Involves implanting a small device that delivers electrical impulses to disrupt pain signals.
- For severe, unrelenting cases, surgical interventions may be considered:
- Conservative Treatments
Self-Care Tips for Managing Occipital Neuralgia
While professional treatments are crucial, lifestyle adjustments can also help manage symptoms:
- Optimize Your Posture: Proper ergonomics at work can prevent strain on your neck and nerves.
- Practice Stress Management: Techniques like yoga, meditation, or deep breathing can reduce tension.
- Stay Active: Gentle physical activity helps keep muscles relaxed and improves circulation.
- Identify Triggers: Certain activities or stressors may worsen your pain. Recognizing these can help you avoid flare-ups.
Living with Occipital Neuralgia
Occipital neuralgia can be frustrating and debilitating, but it doesn’t have to control your life. With the right diagnosis and treatment, most people experience significant improvement. If you’re unsure where to start, consulting a pain management specialist can be a game-changer.
Take the First Step Toward Relief
At Red Butte Pain Solutions, we understand how chronic pain conditions like occipital neuralgia can affect your life. Our team specializes in personalized treatment plans that address your unique needs, helping you reclaim your quality of life. Contact us today at 602-633-4334 to schedule a consultation and take the first step toward a pain-free future.
Occipital headaches: “Ever been stabbed with an ice-pick?”
Occipital headaches are a painful and disruptive condition that affects many people. One of my best friends gets these. He says it feels like he's being stabbed in the back of the head and in the eye with an ice-pick. These headaches cause sharp (like my friend gets)...




