Vertebral Compression Fractures
Broken Back Bones
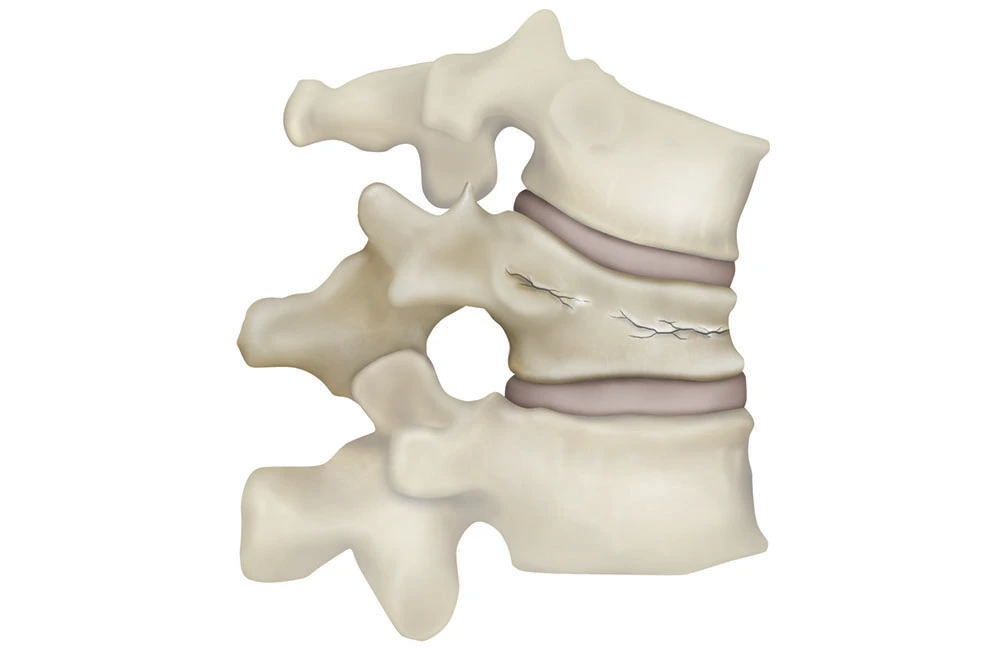
A vertebral compression fracture, often referred to as a “broken back bone,” occurs when one or more of the vertebrae in your spine collapse. This condition can cause significant pain, mobility issues, and even deformity. Understanding the causes, symptoms, diagnosis, and treatment options for vertebral compression fractures is crucial for preventing long-term complications and improving your quality of life.
What Causes Compression Fractures (Broken Back Bones)
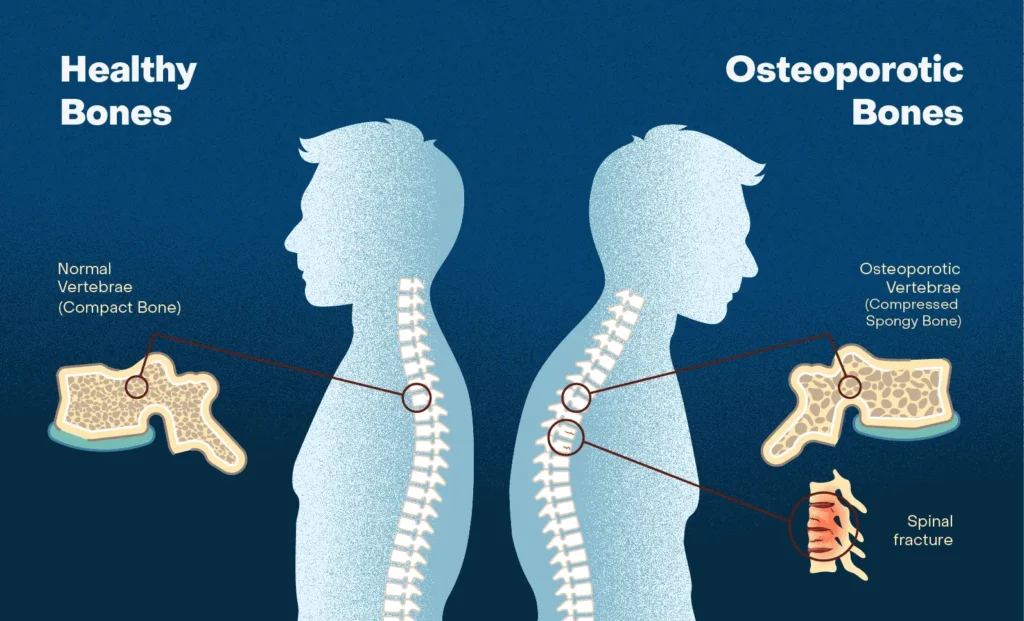
Osteoporosis
Osteoporosis is the leading cause of vertebral compression fractures, often referred to as broken back bones. This condition weakens bones, making them brittle and more prone to fractures, even with minor stress. Among women, 1 in 5 (20 out of 100) have osteoporosis, significantly increasing their risk. Approximately 25% of women in the United States will experience a back fracture in their lifetime, often due to osteoporosis. Post-menopausal women are at the highest risk due to decreased bone density.
Cancer
Certain cancers significantly increase the risk of vertebral compression fractures. Cancers such as multiple myeloma or metastatic cancers (breast, prostate, and lung) can weaken the structural integrity of the spine. When cancer spreads to the vertebrae, it can erode bone tissue, making the spine more susceptible to a broken back bone. Additionally, radiation therapy used to treat spinal metastases can compromise bone integrity, increasing the likelihood of fractures. Studies show that up to 39% of patients who receive radiation for spinal metastases develop vertebral fractures, highlighting the importance of monitoring bone health during and after treatment.
Trauma
While osteoporosis and cancer are common underlying causes, trauma can fracture even healthy vertebrae. High-impact incidents like car accidents, falls, or sports injuries often result in broken back bones, particularly in individuals without underlying conditions.
Other Risk Factors
-
- Chronic steroid use
- Prolonged immobility
- Poor nutrition (lack of calcium and vitamin D)
- Smoking and excessive alcohol consumption
Signs & Symptoms
Acute Back Pain
The most common symptom is sudden, sharp pain in the middle or lower back. This pain is typically localized and may intensify with bending, twisting, or lifting activities. Over time, it can lead to significant limitations in daily activities, as even minor movements might aggravate the discomfort. For some patients, the pain improves with rest, but for others, it may persist and disrupt their ability to sleep, work, or perform routine tasks.
Height Loss
A noticeable decrease in height over time is a hallmark of vertebral compression fractures. This occurs due to collapsing vertebrae.
Spinal (Back) Deformity
Kyphosis, a forward curvature of the spine, may develop as fractures progress, leading to a hunched posture. This characteristic curvature, often seen in elderly individuals, is commonly referred to as a “hunchback.” It results from the collapse of multiple vertebrae over time, which compromises spinal alignment. This posture not only affects appearance but also reduces lung capacity and can impair digestion, further impacting overall health.
Reduced Mobility
Persistent pain and spinal deformity can limit your ability to move, affecting daily activities. This often means difficulty performing basic tasks such as bending, lifting, or walking for extended periods. Over time, these restrictions can lead to decreased independence and a lower quality of life. For elderly individuals, reduced mobility from vertebral fractures increases the risk of falls, further compounding health challenges.
Diagnosing Back Fractures
Medical History and Physical Exam
Your doctor will ask about your symptoms, medical history, and perform a physical exam. They’ll carefully check for signs of a broken back bone, such as tenderness when pressing on specific areas of the spine, reduced ability to bend or twist the back, and visible changes in posture. They may also test for nerve involvement, which can include sensations of numbness, tingling, or weakness in the legs. These findings help identify the severity and potential complications of the fracture, ensuring the right treatment plan is created.
Imaging Tests
-
-
X-rays: Show changes in vertebrae shape, such as wedge-shaped compression or collapsed bones.
-
MRI: Helps identify whether the broken back bone is new or old. Recent fractures often show inflammation (bone marrow edema). MRI is also useful for detecting cancer involvement.
-
DEXA Scans: Measures bone density to assess future fracture risks, including broken back bones and hip fractures.
-
Treatment Options
Conservative Treatments
Pain Medications:
Over-the-counter drugs like acetaminophen or ibuprofen may ease mild pain. Severe pain may require muscle relaxants, such as cyclobenzaprine, to reduce muscle spasms. Opioids may be prescribed for short-term use in cases of intense pain but are used with caution due to the risk of dependency. For persistent or chronic pain, healthcare providers might explore adjunct therapies like nerve-modulating medications to provide more comprehensive relief.
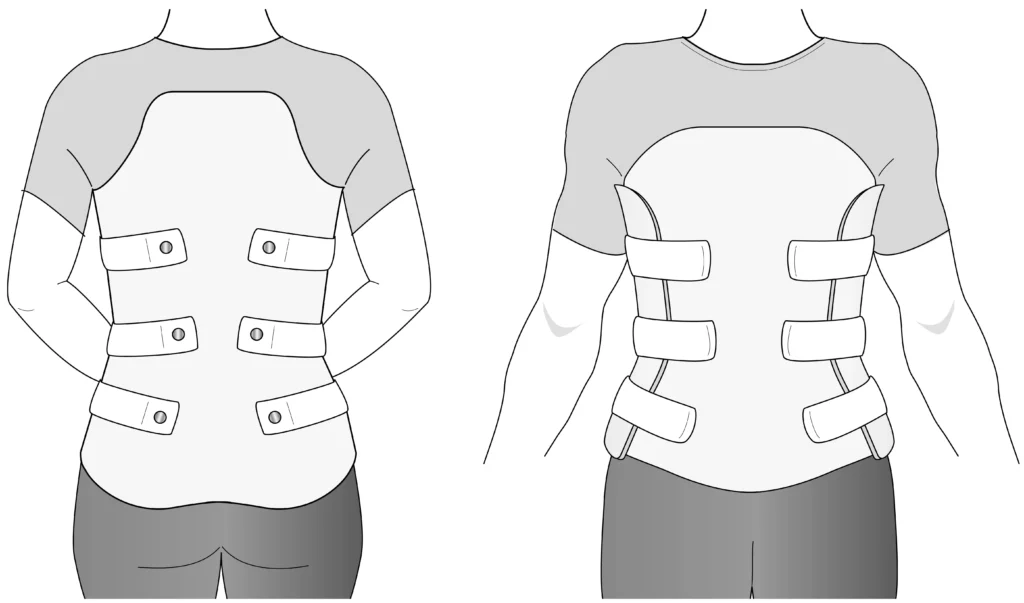
Bracing:
Back braces stabilize the spine and reduce movement, promoting healing. There are different types of braces available, each suited to specific needs:
-
- LSO (Lumbar Sacral Orthosis): Designed to support the lower back, this brace is often used for fractures in the lumbar region. It limits motion while providing stability and reducing pain.
- TLSO (Thoracic Lumbar Sacral Orthosis): This brace supports both the thoracic (mid-back) and lumbar regions. It is commonly prescribed for fractures higher in the spine and provides rigid support to ensure proper healing.
- Clamshell Brace: This rigid brace fully encases the torso, offering maximum stability and immobilization. It is ideal for more severe fractures or patients who require strict motion control.
The primary goal of bracing is to minimize spinal movement, reduce pain, and promote healing of the broken back bone. Most braces are worn for 6-12 weeks, depending on the severity of the fracture and the patient’s progress.
Physical Therapy:
Exercises can improve posture and strengthen the core. Therapy is usually recommended 6-12 weeks after the fracture to ensure proper healing. The goals of physical therapy include improving spinal stability, reducing pain, and enhancing overall mobility. Therapists often focus on strengthening core muscles to provide better support for the spine, improving posture to prevent further complications, and teaching safe movement techniques to avoid reinjury. Physical therapy also helps patients gradually return to daily activities and regain confidence in their physical abilities.

Minimally Invasive Procedures
Minimally invasive procedures offer effective options for treating vertebral compression fractures, often referred to as broken back bones. These procedures are designed to reduce pain, restore function, and improve the quality of life with minimal recovery time compared to traditional surgical approaches. Patients benefit from quicker recovery periods and a lower risk of complications.
-
- Kyphoplasty: This procedure restores vertebral height using a small balloon before stabilizing the fracture with bone cement. It is particularly effective in reducing pain and correcting spinal deformities caused by the fracture. Learn more.
- Vertebroplasty: Similar to kyphoplasty but focuses solely on stabilizing the fracture with bone cement. While it does not restore height, vertebroplasty effectively relieves pain and prevents further collapse. Learn more.
Preventing Future Fractures
Managing Osteoporosis
-
Medications: Bisphosphonates are commonly prescribed to slow bone loss and make bones stronger, reducing the likelihood of a broken back bone. Parathyroid hormone analogues, such as teriparatide and abaloparatide, go a step further by actively stimulating bone growth. These medications are particularly effective for individuals with severe osteoporosis or a history of multiple fractures, helping to rebuild bone density and lower the risk of future broken back bones and other serious complications.
-
Diet: Getting enough calcium and vitamin D supports stronger bones. Calcium is the primary building block for bone strength, while vitamin D helps your body absorb calcium effectively. Without sufficient levels of both, bones can become weak and brittle, increasing the risk of fractures, including a broken back bone. Combining these nutrients in your daily diet through foods like dairy products, leafy greens, and fortified foods, or with supplements if necessary, is essential for maintaining bone health and preventing future injuries.
-
Lifestyle Changes: Quit smoking, limit alcohol, and stay active with weight-bearing exercises.
Monitoring Cancer Patients
Patients with cancer need regular imaging and bone-strengthening treatments to prevent fractures caused by weakened bones. Imaging techniques like X-rays, CT scans, and MRIs are crucial for detecting early signs of bone weakening or fractures. Bone-strengthening treatments, such as bisphosphonates or denosumab, help maintain bone density and reduce the risk of fractures. This proactive approach is essential, as fractures like broken back bones can significantly impact a cancer patient’s quality of life and complicate their overall treatment plan.
Staying Active
Physical activity improves balance and reduces fall risks. Activities like yoga, walking, and tai chi promote bone health and prevent fractures.
Returning Quality to Your Life: Living Well After a Broken Back Bone
Vertebral compression fractures (broken back bones) can significantly affect your quality of life. However, with early diagnosis and proper care, these fractures can be treated effectively. Minimally invasive procedures, such as kyphoplasty and vertebroplasty, offer significant benefits, including pain relief, restored spinal stability, and faster recovery times compared to traditional surgery. At Red Butte Pain Solutions, we specialize in these advanced treatments, tailoring each care plan to your unique needs. Don’t let a broken back bone hold you back—call 602-633-4334 today to schedule a consultation and take the first step toward recovery and renewed mobility.
Call 602-633-4334 or Click Below
Middle Back Bone Pain: Causes and Treatment Options
Middle back bone pain can come from arthritis, fractures, or cancer. Learn what’s causing your pain and how Red Butte Pain Solutions can help.
Vertebral Compression Fracture Treatment Options for Pain Relief
Vertebral compression fractures (VCFs) affect over 700,000 Americans each year. These small spine fractures, often due to osteoporosis, trauma, or cancer, can cause intense pain and disability. Fortunately, several vertebral compression fracture treatment options can...
What Causes Aching Pain Between the Shoulder Blades?
Aching pain between the shoulder blades is a common complaint that often comes and goes. But sometimes, it can be a sign of something more serious. Understanding the potential causes can help you get the right treatment. Common Causes of Aching Pain Between the...
How Much Does A Broken Back Cost?
Over the course of my career, I've watched how the broken back cost has become a growing concern—not just for insurance companies, but for patients themselves. With rising co-pays, co-insurances, and out-of-pocket expenses, patients now bear a much larger share of the...
Treatment for Broken Back Vertebra
A broken back vertebra, also known as a [vertebral compression fracture, can cause sudden, severe pain and significantly limit daily activities. These fractures are most often due to weakened bones from osteoporosis. Prompt treatment can ease pain, promote healing,...
When Back Pain Means More: Back Pain From Cancer
Back pain is common. But sometimes, it's more than a pulled muscle or a slipped disc. In some cases, back pain can be a warning sign of cancer. At Red Butte Pain Solutions, we help patients understand the cause of their pain. If you or a loved one has back pain and a...
Is a TLSO Back Brace Right for Me?
A TLSO back brace (thoracolumbosacral orthosis) is a rigid brace designed to stabilize the thoracic and lumbar spine. This provides essential support for individuals recovering from injuries, helps in managing chronic pain, and correcting postural issues. These braces...
Suffering from a Sacral Fracture? Learn Symptoms, Causes, and Treatments
As a specialized pain management practice, we frequently treat patients with sacral fractures. A sacral fracture is a break in the sacrum, the triangular bone at the base of the spine. These fractures can cause significant pain and mobility issues, affecting daily...
Back Bracing: Will It Work For Me?
Back bracing is a frequent topic of discussion at Red Butte Pain Solutions. For example, nearly 70% of patients with vertebral compression fractures report significant pain relief when using a brace, highlighting its importance in recovery and pain management. Many...
Can Prostate Cancer Cause Back Pain?
As a pain management physician, I often hear the question, “Doc, can prostate cancer cause back pain?” The short answer is yes, prostate cancer can cause back pain. However, it’s crucial to understand that back pain has many causes, and most of the time, the...