Post Laminectomy Syndrome
Post Laminectomy Syndrome: Getting to Better
 So, you had back surgery to relieve pain and get your life back. But instead of relief, you’re still struggling with pain—or maybe it’s even worse. This is what we call post laminectomy syndrome (PLS) or failed back surgery syndrome (FBSS), and if you’re experiencing it, you’re not alone. At Red Butte Pain Solutions, we’re here to help you find real answers and solutions.
So, you had back surgery to relieve pain and get your life back. But instead of relief, you’re still struggling with pain—or maybe it’s even worse. This is what we call post laminectomy syndrome (PLS) or failed back surgery syndrome (FBSS), and if you’re experiencing it, you’re not alone. At Red Butte Pain Solutions, we’re here to help you find real answers and solutions.
What Is Post Laminectomy Syndrome?
Let’s start with the basics. Post laminectomy syndrome is chronic pain that continues—or starts—after back surgery. It might feel like the same pain you had before surgery or a new type of discomfort. Either way, it’s incredibly frustrating, especially when you’ve gone through surgery hoping to finally feel better.
Common symptoms include:
- Pain in your lower back or neck
- Pain that shoots down your legs or arms (like sciatica)
- Numbness, tingling, or weakness
- Pain that gets worse when you sit, stand, or move
- Trouble sleeping because of the pain
If this sounds familiar, know that there’s hope. With the right approach, we can help you get back to living.
How Common Is Post Laminectomy Syndrome?
You might be surprised to learn how many people go through this. Studies show that about 20% of people who have back surgery end up with post laminectomy syndrome. That means one out of five patients who go through surgery might still deal with significant pain afterward. You’re not alone, and it’s not your fault.
Causes of Post Laminectomy Syndrome
Why Does Post Laminectomy Syndrome Happen?
PLS doesn’t happen because you did something wrong or your surgeon made a mistake. It’s often a mix of natural healing processes and the spine’s complexity. Here are a few common causes:
- Scar Tissue: Surgery can lead to scar tissue that irritates nearby nerves.
- Recurring Disc Issues: A new herniation near the surgical site can cause pain similar to what you had before.
- Nerve Damage: Nerves affected by your initial condition or surgery might not fully recover, leading to ongoing nerve pain.
- Adjacent Segment Disease: Fusion surgery, while helpful, can increase wear and tear on the levels above or below the fused area. This can lead to new pain from degeneration in those areas.
- Facet Joint Problems: Spinal surgery can put more strain on the facet joints, leading to arthritis or inflammation.
- Spinal Instability: Fusion surgeries may sometimes lead to instability in other spinal areas.
- Inadequate Decompression: Remaining pressure on spinal nerves after surgery.
Understanding the “why” behind your pain helps us target it with the right treatments.
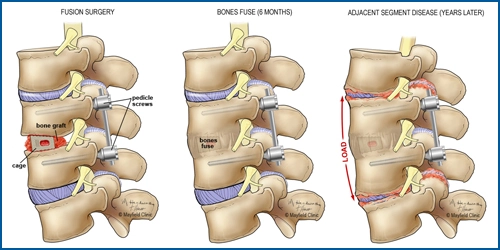
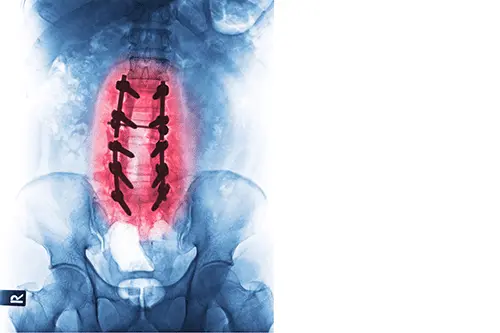
Impact of Spinal Fusion on Adjacent Segment Degeneration and Facet Arthropathy
Spinal fusion, while effective in stabilizing specific spinal segments, can inadvertently accelerate degeneration in adjacent segments. This phenomenon, known as adjacent segment degeneration (ASD), occurs due to increased biomechanical stress on the levels above or below the fused segment.
ASD can manifest as:
- Facet Joint Arthropathy: Degeneration of the facet joints, leading to pain and reduced mobility.
- Disc Degeneration: Accelerated wear and tear of intervertebral discs adjacent to the fusion site.
- Spinal Stenosis: Narrowing of the spinal canal, potentially compressing nerve roots.
Understanding these potential complications underscores the need for careful surgical planning and postoperative monitoring to mitigate the risks associated with spinal fusion.
Diagnosing Post Laminectomy Syndrome
Getting to the Root of Your Pain
Finding relief starts with understanding exactly what’s causing your pain. Post laminectomy syndrome isn’t one-size-fits-all—it can come from different problems, like scar tissue, nerve damage, or new issues in the spine. Accurate diagnosis is the cornerstone of effective treatment for post laminectomy syndrome (PLS). At Red Butte Pain Solutions, we are committed to identifying the underlying causes of your pain to tailor treatments that align with the latest evidence-based practices. Understanding that PLS can result from a variety of structural, neurological, or biomechanical issues, we employ a meticulous and collaborative diagnostic process.
A Multi-Faceted Evaluation to Pinpoint the Cause
Diagnosing PLS requires exploring multiple potential contributors to your pain. These may include residual nerve compression, scar tissue, joint degeneration, or adjacent segment disease. Our approach combines patient history, physical examinations, and advanced diagnostics to uncover the root cause.
Diagnosing the Causes of Post Laminectomy Syndrome Involves:
-
- Comprehensive Medical History and Physical Exam: Let’s Talk About Your Pain
- We begin with a detailed discussion of your symptoms, surgery history, and current challenges. When did the pain start? What does it feel like? What treatments have (or haven’t) worked so far? Your story is crucial in figuring out the next steps.
- A thorough physical exam helps assess your pain patterns, mobility, and neurological function.
- Advanced Imaging Techniques
- MRI or CT Scans: Identify structural issues like recurrent disc herniation, scar tissue, or spinal stenosis.
- X-rays with Movement: Flexion and extension X-rays show us how stable your spine is when you move.
- Electrodiagnostic Testing
- Nerve Conduction Studies (NCS) and Electromyography (EMG): Diagnose nerve damage or dysfunction that may contribute to your pain.
- Diagnostic Injections
- Nerve Blocks: Temporarily anesthetize specific nerves to confirm their involvement in your pain.
- Facet Joint or Epidural Injections: Help isolate pain sources in the spine.
- Comprehensive Medical History and Physical Exam: Let’s Talk About Your Pain
Treatment for Post Laminectomy Syndrome
When it comes to managing PLS, there’s no single solution that works for everyone. That’s why we take the time to really understand your pain and its underlying causes. From cutting-edge treatments to lifestyle tweaks, we build a plan that’s just for you.
Medications: A Helpful First Step
Medications can be a great starting point for managing your symptoms. They don’t cure the problem, but they can help control inflammation, nerve pain, and muscle spasms.
- Anti-Inflammatories: These reduce swelling and help you feel more comfortable.
- Nerve Pain Medications: Medications like gabapentin and duloxetine target nerve-related pain.
- Muscle Relaxants: If muscle spasms are part of the problem, these can bring some relief.
- Short-Term Opioids: For severe pain, we may use these carefully and only when absolutely necessary.
We’ll work with you to find the right combination, ensuring you get relief without unnecessary side effects.
Physical Therapy: Get Moving Again
Think of physical therapy as hitting the reset button for your body. The right exercises can rebuild strength, improve flexibility, and help you move without triggering pain.
- Strengthening Exercises: Build up those core and spinal muscles to protect your back.
- Stretching: Relieve tightness and improve mobility.
- Postural Training: Learn how to move and sit in ways that don’t stress your spine.
- Hands-On Techniques: Massage or other manual therapies can ease tension and improve how your body feels.
Physical therapy isn’t just about exercises—it’s about getting your body back to feeling like your own.
Injections for Targeted Relief
Sometimes, the quickest way to get relief is to go straight to the source of the pain. That’s where injections come in.
- Epidural Steroid Injections: These reduce inflammation and swelling around irritated nerves, offering relief from sciatica or radicular pain.
- Nerve Blocks: These temporary numbing injections not only relieve pain but also help us pinpoint its exact source.
- Facet Joint Injections: If arthritis in the joints of your spine is to blame, this can provide relief.
Injections are often a game-changer, giving you enough relief to get back to physical therapy or other activities.
Radiofrequency Ablation: Long-Lasting Relief
If arthritis in your spine’s facet joints is causing pain, radiofrequency ablation (RFA) could be the answer. This procedure uses heat to deactivate the nerves that send pain signals from these joints. It’s minimally invasive, and the relief can last from six months to over a year. Imagine finally being able to move without that constant, nagging pain.
Spinal Cord Stimulation: Rewiring How You Feel Pain
For chronic nerve pain that just won’t quit, spinal cord stimulation (SCS) offers a high-tech solution. Think of it as a pain interrupter: a small device sends electrical signals to your spinal cord, stopping pain signals from reaching your brain. And here’s the best part—you get to try it out first with a temporary device to see if it works for you.
Many patients say their quality of life improves dramatically with SCS, allowing them to cut back on medications and get back to the things they love.
Lifestyle Changes: Small Adjustments, Big Impact
Sometimes, the little things make the biggest difference. That’s why we emphasize lifestyle changes to help you manage your pain every day.
- Weight Management: Less weight means less strain on your spine.
- Ergonomic Tweaks: Simple changes at your desk or home can keep your back in better alignment.
- Mind-Body Techniques: Yoga, mindfulness, and meditation help manage the stress and emotional toll of chronic pain.
We’ll guide you in making these changes, so they feel manageable and, more importantly, effective.
Why Choose Red Butte Pain Solutions?
At Red Butte Pain Solutions, our team understands the frustration of unresolved pain after back surgery. We work closely with you to create a treatment plan tailored to your needs and goals. With our expertise in interventional pain management, we aim to provide lasting relief and help you regain control of your life.
Let’s Take the Next Step Together
Don’t let post laminectomy syndrome or failed back surgery syndrome keep holding you back. Relief is possible, and we’re here to help you find it. Call us today at 602-633-4334 or request an appointment online. Let’s work together to get you moving and feeling better again. You’ve got this—and we’ve got you.
Do Stims Stim? The HFX Spinal Cord Stimulator
Introduction At Red Butte Pain Solutions, we’re always exploring new options for effective pain relief, including spinal cord stimulator (SCS) devices. Many of you may have read our recent post on Differential Targeted Multiplex (DTM) stimulation, where we covered its...
Breaking New Ground in Pain Management: DTM and Closed-Loop Spinal Cord Stimulation
When I was in training, I was taught that "Stims stim," meaning there wasn’t much difference between spinal cord stimulation (SCS) devices beyond customer service for our patients. Back then, no SCS devices had MRI compatibility, and the only real debate was whether...
Adjacent Segment Disease: A Patient’s Journey
The Sciatica Strikes Back A few weeks ago, a patient came to Red Butte Pain Solutions with severe lower back and leg pain. Years earlier, he had undergone surgery for a herniated disc. After the surgery, he felt better and lived pain-free. But now, the pain had...

