Back Pain
Lumbar Radiculopathy
Lumbar Radiculopathy: Causes, Symptoms, and Treatment Options
Introduction
Lumbar radiculopathy, often referred to as sciatica, is a common cause of back and leg pain. It occurs when nerve roots in the lumbar spine become compressed, leading to symptoms like pain, numbness, and weakness in the lower back, buttocks, and legs. At Red Butte Pain Solutions, we specialize in helping patients find relief from this condition. If you’re experiencing persistent back pain, understanding lumbar radiculopathy can be the first step toward finding effective treatment. This article will guide you through the causes, symptoms, and treatment options for lumbar radiculopathy, helping you make informed decisions about your care.
Understanding Lumbar Radiculopathy
Lumbar radiculopathy happens when a nerve in the lower spine is pinched or irritated. The lumbar spine consists of five vertebrae located in the lower back, supporting much of the body’s weight. Between each vertebra, there are discs that act as cushions, absorbing shocks and allowing movement. Nerve roots branch out from the spinal cord at every vertebra. When a disc herniates or degenerates, it can press against these nerves, causing pain and discomfort.
Causes of Lumbar Radiculopathy
Several conditions can cause lumbar radiculopathy, with the most common being:
- Herniated Discs
A herniated disc occurs when the soft inner material of a spinal disc pushes through its outer layer. This material can press against nearby nerves, causing pain that radiates down the leg. Herniated discs are common in the lower back and are a leading cause of lumbar radiculopathy. - Degenerative Disc Disease
As we age, spinal discs can lose hydration and elasticity. This natural process, known as degenerative disc disease, weakens the discs and can lead to nerve compression. The result is often persistent lower back pain and sciatica. - Spinal Stenosis
Spinal stenosis is the narrowing of the spinal canal, which puts pressure on the nerves. It’s more common in older adults and can cause both lumbar radiculopathy and lower back pain. The condition tends to worsen over time without treatment. - Spondylolisthesis
Spondylolisthesis occurs when one vertebra slips forward over another, narrowing the space for the nerves. This misalignment can lead to nerve root compression and sciatica. The condition can be caused by age-related wear or trauma. - Trauma
Injuries to the spine, such as fractures or dislocations, can lead to lumbar radiculopathy. Trauma may damage the discs or bones in the lumbar spine, resulting in nerve compression.
Symptoms of Lumbar Radiculopathy
The hallmark symptom of lumbar radiculopathy is pain that radiates from the lower back into the leg. This pain, often called sciatica, follows the path of the sciatic nerve, which runs from the lower spine to the foot. Other common symptoms include:
- Lower Back Pain
Patients with lumbar radiculopathy often experience dull, aching pain in the lower back. The pain may be constant or worsen with certain activities, like bending, lifting, or sitting for extended periods. - Leg Pain
Pain that shoots down one leg is a defining feature of sciatica. The pain may feel sharp, burning, or electric-like and can extend all the way to the foot. - Numbness or Tingling
Lumbar radiculopathy may cause numbness or tingling in the affected leg or foot. Patients often report feeling pins and needles in the areas where the nerve is compressed. - Weakness
In severe cases, lumbar radiculopathy can lead to muscle weakness. This weakness usually affects the leg or foot and can make walking or standing difficult. - Loss of Reflexes
Reflexes in the knee or ankle may be diminished in patients with lumbar radiculopathy. This can be detected during a physical exam by a healthcare provider.
Diagnosis of Lumbar Radiculopathy
Accurate diagnosis of lumbar radiculopathy is essential for effective treatment. At Red Butte Pain Solutions, we take a comprehensive approach to diagnosing this condition. The diagnostic process typically involves:
- Medical History
Your provider will ask about your symptoms, including the location, severity, and duration of your pain. They may also ask about any previous injuries or medical conditions that could contribute to your symptoms. - Physical Examination
A thorough physical exam helps identify signs of nerve compression. Your provider will test your muscle strength, reflexes, and ability to perform certain movements. - Imaging Tests
Imaging tests, such as X-rays, MRI scans, or CT scans, may be used to visualize the spine and identify the exact location of nerve compression. These tests are essential for pinpointing the cause of lumbar radiculopathy. - Nerve Conduction Studies
In some cases, nerve conduction studies or electromyography (EMG) may be performed to assess the function of the nerves and muscles. These tests measure the electrical activity in the muscles and can help determine the extent of nerve damage.
Treatment Options for Lumbar Radiculopathy
At Red Butte Pain Solutions, we offer a range of treatment options for lumbar radiculopathy. Our goal is to relieve pain, improve function, and prevent future nerve damage. Treatment options include:
Conservative Treatment
Most cases of lumbar radiculopathy improve with conservative treatments. These include:
-
- Rest and Activity Modification
Avoiding activities that worsen your symptoms, such as heavy lifting or prolonged sitting, can help reduce nerve irritation. Bed rest is not recommended, but limiting strenuous activities can provide relief. - Physical Therapy
Physical therapy can help strengthen the muscles in your lower back, improve flexibility, and reduce pressure on the nerves. A tailored exercise program can help you return to normal activities. - Medications
Over-the-counter pain relievers, like ibuprofen or acetaminophen, may provide temporary relief. In some cases, prescription medications, such as muscle relaxants or nerve pain medications, may be recommended. - Epidural Steroid Injections
Epidural steroid injections deliver anti-inflammatory medication directly to the area around the irritated nerve. These injections can provide significant relief from pain and inflammation and are often used when conservative treatments have not been effective.
- Rest and Activity Modification
Surgical Treatment
If conservative treatments fail to relieve symptoms or if the nerve compression is severe, surgery may be necessary. Surgical options include:
-
- Discectomy
A discectomy involves removing the portion of a herniated disc that is pressing on the nerve. This procedure can quickly relieve sciatica and improve mobility. - Laminectomy
A laminectomy involves removing part of the vertebra to relieve pressure on the nerves. This surgery is often performed in cases of spinal stenosis. - Spinal Fusion
In some cases, spinal fusion surgery may be recommended to stabilize the spine and prevent further nerve damage. This procedure involves fusing two or more vertebrae together.
- Discectomy
Preventing Lumbar Radiculopathy
While lumbar radiculopathy can be treated, taking steps to prevent future episodes is important. Here are some tips to reduce your risk of developing this condition:
- Maintain a Healthy Weight
Excess body weight puts added stress on the lower back, increasing the risk of lumbar radiculopathy. Maintaining a healthy weight through diet and exercise can help protect your spine. - Exercise Regularly
Regular exercise helps strengthen the muscles that support the spine and improve flexibility. Focus on exercises that strengthen your core, such as swimming, walking, or yoga. - Use Proper Lifting Techniques
Avoid lifting heavy objects with your back. Instead, bend at the knees and use your legs to lift. This reduces the strain on your lower back. - Practice Good Posture
Sitting or standing with poor posture can strain your lower back over time. Be mindful of your posture, especially when sitting for long periods. Use ergonomic chairs and maintain a neutral spine position.
When to Seek Medical Attention
If you experience persistent back or leg pain, it’s important to seek medical attention. Lumbar radiculopathy can worsen over time if left untreated, leading to more severe symptoms. Contact Red Butte Pain Solutions if you experience:
- Pain that radiates down one leg
- Numbness or tingling in the leg or foot
- Muscle weakness in the leg or foot
- Difficulty walking or standing
- Loss of bladder or bowel control (This is a medical emergency)
Conclusion
Lumbar radiculopathy, or sciatica, is a common condition that can cause significant pain and discomfort. Understanding the causes, symptoms, and treatment options can help you take control of your condition and find relief. At Red Butte Pain Solutions, we are committed to providing effective, personalized care for patients suffering from back pain in Arizona. Whether through conservative treatments or advanced procedures, we’re here to help you return to a pain-free life.
If you’re experiencing lumbar radiculopathy, don’t wait. Contact Red Butte Pain Solutions today for a consultation and begin your journey to lasting relief.
Is Piriformis Syndrome Curable? – The Best Exercises and Stretches for Relief
What is Piriformis Syndrome? Piriformis syndrome is a common but often overlooked cause of buttock and leg pain, affecting an estimated 6% of patients diagnosed with sciatica. It occurs when the piriformis muscle, located deep in the buttock, compresses or irritates...
The Connection Between Hip Pain and Back Pain
When I was a kid, there was a song called "The Skeleton Dance" where we sang, "The foot bone's connected to the leg bone. The leg bone's connected to the knee bone..." and so on. This simple, catchy tune shows how the body’s structures are biomechanically connected. I...
Deep Dive: Transforaminal Epidural Steroid Injection
One of the most frequent injections I perform is a transforaminal epidural steroid injection. I'm often asked by patients, particularly women, "Is this like an epidural when you have a baby?" And I get to explain that it's really something altogether different. If...
Epidural Steroid Injections: Isn’t This Just a Band-Aid?
Epidural steroid injections are one of the most common procedures I perform. This is in no small part due to the fact that every year one of the top reasons people see a doctor is back pain. Patients often have questions like, “How does the steroid work to stop the...
Adjacent Segment Disease: A Patient’s Journey
The Sciatica Strikes Back A few weeks ago, a patient came to Red Butte Pain Solutions with severe lower back and leg pain. Years earlier, he had undergone surgery for a herniated disc. After the surgery, he felt better and lived pain-free. But now, the pain had...
From Pain to Relief: Treating Lumbar Disc Herniation in Arizona
At Red Butte Pain Solutions, we see patients with various types of back pain. One common condition we treat is lumbar disc herniation, including disc extrusions. A disc extrusion occurs when the soft inner material of a disc in the spine pushes through a tear in the...
Back Pain: Finding Causes and Effective Back Pain Relief
Back pain is a common issue that affects millions of people each year. Back pain can range from mild discomfort to severe, chronic pain that disrupts daily life. While simple remedies like stretching or massage offer relief for many, these solutions may only provide...
Call us at 602-633-4334 or Click Below
Spinal Stenosis
Understanding Lumbar Stenosis Back Pain
Are you a resident of Chandler, Mesa, Ahwatukee, Sun Lakes, Tempe, Gilbert, Phoenix, Maricopa, or Casa Grande, Arizona, and experiencing back or leg pain that worsens with standing and walking? You might be dealing with a condition known as lumbar spinal stenosis.
What is Lumbar Spinal Stenosis?
Lumbar spinal stenosis is a condition where the spinal canal in your lower back, or lumbar region, narrows. This narrowing can put pressure on your spinal cord and the nerves that travel through the spine to your legs.
Signs and Symptoms
One common symptom of lumbar spinal stenosis is pain in the back and legs that worsens when standing and walking, a condition often referred to as the “shopping cart sign”. This term comes from the observation that people with this condition often find relief when leaning forward, such as when pushing a shopping cart.
Other symptoms may include:
- Numbness or tingling in your foot or leg
- Weakness in your foot or leg
- Loss of balance
- Lower back pain when standing or walking
Managing Lumbar Spinal Stenosis
At Red Butte Pain Solutions, we specialize in providing comprehensive, individualized treatment plans for conditions like lumbar spinal stenosis. Our goal is to help you manage your symptoms and improve your quality of life.
Remember, it’s important to consult with a healthcare professional if you’re experiencing any of these symptoms. Early diagnosis and treatment can help prevent further damage and manage symptoms more effectively.
Treatment Options
At Red Butte Pain Solutions, we offer a variety of treatments for lumbar spinal stenosis. Two of the most effective treatments are epidural steroid injections and spinal cord stimulation.
Epidural Steroid Injections
Epidural steroid injections involve injecting a steroid medication into the epidural space of your spine. This can help reduce inflammation and relieve pain. It’s a minimally invasive procedure that can provide significant relief for many patients.
Spinal Cord Stimulation
For more severe cases, spinal cord stimulation might be an option. This involves implanting a device that sends low-level electrical signals to the spinal cord or specific nerves to block pain signals from reaching the brain. This treatment can help manage chronic pain conditions, such as lumbar spinal stenosis.
Prevention
While it’s not always possible to prevent lumbar spinal stenosis, there are steps you can take to reduce your risk and slow its progression:
- Maintain a healthy weight
- Regular exercise
- Practice good posture
- Regular check-ups with your healthcare provider
Remember, it’s important to consult with a healthcare professional for a proper diagnosis and treatment plan. At Red Butte Pain Solutions, we’re here to help you navigate your journey to pain relief.
This content is intended for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment.
What Causes Aching Pain Between the Shoulder Blades?
Aching pain between the shoulder blades is a common complaint that often comes and goes. But sometimes, it can be a sign of something more serious. Understanding the potential causes can help you get the right treatment. Common Causes of Aching Pain Between the...
Deep Dive: Transforaminal Epidural Steroid Injection
One of the most frequent injections I perform is a transforaminal epidural steroid injection. I'm often asked by patients, particularly women, "Is this like an epidural when you have a baby?" And I get to explain that it's really something altogether different. If...
Epidural Steroid Injections: Isn’t This Just a Band-Aid?
Epidural steroid injections are one of the most common procedures I perform. This is in no small part due to the fact that every year one of the top reasons people see a doctor is back pain. Patients often have questions like, “How does the steroid work to stop the...
Adjacent Segment Disease: A Patient’s Journey
The Sciatica Strikes Back A few weeks ago, a patient came to Red Butte Pain Solutions with severe lower back and leg pain. Years earlier, he had undergone surgery for a herniated disc. After the surgery, he felt better and lived pain-free. But now, the pain had...
From Pain to Relief: Treating Lumbar Disc Herniation in Arizona
At Red Butte Pain Solutions, we see patients with various types of back pain. One common condition we treat is lumbar disc herniation, including disc extrusions. A disc extrusion occurs when the soft inner material of a disc in the spine pushes through a tear in the...
Spinal Stenosis: Pathways to Relief
Spinal stenosis is a common condition that affects many people, especially as they age. If you're experiencing back pain and are unsure of the cause, it might be due to spinal stenosis. At Red Butte Pain Solutions in Chandler, Arizona, we specialize in diagnosing and...
Facet Arthritis
Related Topics:
Facet Arthritis: Understanding and Managing Back Pain
Introduction
Facet arthritis is a common cause of chronic back pain, affecting millions of people worldwide. This condition occurs when the small joints in the spine, called facet joints, become inflamed or damaged. Over time, this leads to pain, stiffness, and reduced mobility. At Red Butte Pain Solutions, we specialize in treating facet arthritis to help patients regain their quality of life. If you’re suffering from back pain and suspect arthritis may be the cause, understanding facet arthritis is essential. In this article, we will explore what facet arthritis is, its causes, symptoms, diagnosis, and treatment options.
What is Facet Arthritis?

Facet arthritis, also known as facet joint osteoarthritis, is the breakdown of cartilage within the facet joints of the spine. The facet joints are small, stabilizing joints located at the back of each vertebra. These joints allow your spine to move smoothly, enabling you to twist, bend, and arch your back. When the cartilage in these joints wears down, the bones can rub against each other, leading to pain, swelling, and stiffness.
Facet arthritis commonly affects the cervical (neck) and lumbar (lower back) regions of the spine. It often results in localized pain, but it can also cause pain that radiates to other parts of the body, including the shoulders, buttocks, or legs. The condition typically worsens with age but can also develop due to injury or overuse.
Causes of Facet Arthritis
Facet arthritis can develop due to several factors. Some of the most common causes include:
Aging
As you age, the cartilage in your facet joints naturally wears down. This process is called degeneration. Over time, this degeneration can lead to arthritis. Most people over the age of 60 have some degree of facet arthritis, even if they don’t experience symptoms.
Wear and Tear
Repetitive movements and overuse can speed up the breakdown of cartilage in the facet joints. People who perform heavy physical labor or high-impact sports are at a higher risk of developing facet arthritis.
Spinal Injury
Trauma to the spine, such as from a car accident or fall, can damage the facet joints. Injuries can cause the cartilage to deteriorate faster, leading to early-onset arthritis.
Spinal Misalignment
Conditions that cause the spine to be misaligned, such as scoliosis or spondylolisthesis, can increase stress on the facet joints. Over time, this extra pressure can lead to arthritis.
Obesity
Carrying excess weight places extra stress on the spine, especially on the facet joints in the lower back. This added pressure can accelerate the breakdown of cartilage and lead to facet arthritis.
Previous Spinal Surgery
Some individuals who have had spinal surgery, such as a laminectomy or fusion, may develop facet arthritis in the years following the procedure. This is due to changes in the mechanics of the spine.
Symptoms of Facet Arthritis
The symptoms of facet arthritis vary depending on the location of the affected joints and the severity of the condition. Common symptoms include:
-
- Back Pain
The primary symptom of facet arthritis is localized pain in the affected region of the spine. For lumbar facet arthritis, pain is typically felt in the lower back. For cervical facet arthritis, pain occurs in the neck and shoulders. The pain is often described as a deep, dull ache that worsens with certain movements. - Stiffness
Facet arthritis can cause stiffness in the back, especially in the morning or after periods of inactivity. Stiffness may make it difficult to bend, twist, or rotate the spine. - Pain with Movement
Movements such as twisting, bending backward, or arching the spine can aggravate the facet joints, leading to increased pain. Pain may also worsen after prolonged periods of standing or sitting. - Radiating Pain
In some cases, facet arthritis causes referred pain that radiates to other areas. Lumbar facet arthritis can lead to pain in the buttocks or thighs, while cervical facet arthritis may cause pain in the shoulders or upper arms. - Muscle Spasms
Facet arthritis can lead to muscle spasms or tightness in the surrounding muscles as they work to stabilize the spine.
- Back Pain
Diagnosing Facet Arthritis
At Red Butte Pain Solutions, our team uses a thorough approach to diagnose facet arthritis. The diagnostic process typically includes:
-
- Medical History
Your provider will ask about your symptoms, including the location, intensity, and duration of your pain. They may also inquire about any previous injuries, surgeries, or medical conditions that could contribute to arthritis. - Physical Examination
During a physical exam, your provider will assess your range of motion, strength, and flexibility. They may perform specific movements to pinpoint areas of tenderness and stiffness in the spine. - Imaging Tests
Imaging tests such as X-rays, MRI scans, or CT scans are often used to visualize the facet joints and detect signs of arthritis. These tests can reveal joint space narrowing, bone spurs, or cartilage loss, which are indicative of facet arthritis. - Diagnostic Injections
In some cases, a diagnostic injection may be used to confirm the source of the pain. Your provider may inject a local anesthetic into the suspected facet joint. If your pain improves after the injection, it is likely that facet arthritis is the cause.
- Medical History
Treatment Options for Facet Arthritis
Facet arthritis can be managed through a combination of non-surgical and surgical treatments. At Red Butte Pain Solutions, we offer a wide range of treatments to help you find relief from facet arthritis. Common treatments include:
Conservative Management
Many patients find relief from conservative treatments, which focus on reducing pain and improving mobility. These include:
-
- Physical Therapy
Physical therapy is often recommended to strengthen the muscles that support the spine and improve flexibility. Your physical therapist will guide you through exercises designed to stabilize the spine and reduce stress on the facet joints. - Medications
Over-the-counter pain relievers, such as acetaminophen or ibuprofen, can help manage the pain and inflammation caused by facet arthritis. In some cases, prescription medications may be necessary. - Heat and Cold Therapy
Applying heat or ice packs to the affected area can help relieve pain and reduce inflammation. Heat helps relax muscles and improve blood flow, while cold therapy can numb the area and reduce swelling. - Lifestyle Changes
Making lifestyle changes, such as maintaining a healthy weight, practicing good posture, and avoiding activities that strain the spine, can help prevent the progression of facet arthritis.
- Physical Therapy
Interventional Pain Management
For patients with moderate to severe facet arthritis, interventional pain management techniques may provide relief. These treatments target the source of the pain directly and are often used when conservative methods fail to provide sufficient relief.
-
- Facet Joint Injections
Facet joint injections involve injecting a mixture of local anesthetic and corticosteroid directly into the affected joint. The anesthetic provides immediate pain relief, while the corticosteroid reduces inflammation and swelling. - Radiofrequency Ablation
Radiofrequency ablation (RFA) is a minimally invasive procedure that uses heat to destroy the nerves that transmit pain signals from the facet joints. This procedure can provide long-term relief from facet arthritis, typically lasting six months to a year.
- Facet Joint Injections
Surgical Options
Surgery is rarely needed for facet arthritis, but it may be recommended if conservative and interventional treatments fail to provide relief. Surgical options include:
-
- Facet Joint Fusion
Facet joint fusion involves surgically fusing two vertebrae together to eliminate movement in the affected joint. This procedure stabilizes the spine and can help reduce pain from facet arthritis. - Laminectomy
In some cases, a laminectomy may be performed to remove part of the vertebra and relieve pressure on the nerves. This procedure is often used when facet arthritis causes nerve compression or spinal stenosis.
- Facet Joint Fusion
Preventing Facet Arthritis
While facet arthritis cannot always be prevented, there are steps you can take to reduce your risk and protect your spine:
-
- Maintain a Healthy Weight
Carrying excess weight puts additional stress on the spine and increases your risk of developing facet arthritis. Maintaining a healthy weight can help preserve the health of your facet joints. - Stay Active
Regular exercise strengthens the muscles that support your spine and improves flexibility. Low-impact activities like swimming, walking, or yoga are excellent for maintaining spinal health. - Use Proper Posture
Poor posture places extra stress on the spine, increasing the risk of facet arthritis. Practice good posture when sitting, standing, and lifting to protect your spine. - Avoid Repetitive Movements
Repetitive movements that strain your spine can lead to facet arthritis over time. If your job or daily activities require repetitive motions, take frequent breaks and use proper body mechanics.
- Maintain a Healthy Weight
Conclusion
Facet arthritis is a leading cause of chronic back pain that can significantly impact your quality of life. Understanding the causes, symptoms, and treatment options can help you manage the condition and find relief. At Red Butte Pain Solutions, we offer comprehensive care for patients with facet arthritis in Arizona. Whether you’re looking for conservative treatments or advanced interventional procedures, our team is here to help.
If you’re experiencing persistent back pain and suspect facet arthritis, contact Red Butte Pain Solutions at 602-633-4334 today to schedule a consultation. We’re committed to helping you find the relief you deserve.
Middle Back Bone Pain: Causes and Treatment Options
Middle back bone pain can come from arthritis, fractures, or cancer. Learn what’s causing your pain and how Red Butte Pain Solutions can help.
What Causes Aching Pain Between the Shoulder Blades?
Aching pain between the shoulder blades is a common complaint that often comes and goes. But sometimes, it can be a sign of something more serious. Understanding the potential causes can help you get the right treatment. Common Causes of Aching Pain Between the...
The Connection Between Hip Pain and Back Pain
When I was a kid, there was a song called "The Skeleton Dance" where we sang, "The foot bone's connected to the leg bone. The leg bone's connected to the knee bone..." and so on. This simple, catchy tune shows how the body’s structures are biomechanically connected. I...
Radiofrequency Ablation: Relief for Chronic Pain
At Red Butte Pain Solutions, radiofrequency ablation (RFA) is one of our most effective tools for treating chronic pain. This minimally invasive procedure uses heat generated by radio waves to target specific nerves and disrupt their ability to transmit pain signals....
Back Pain: Finding Causes and Effective Back Pain Relief
Back pain is a common issue that affects millions of people each year. Back pain can range from mild discomfort to severe, chronic pain that disrupts daily life. While simple remedies like stretching or massage offer relief for many, these solutions may only provide...
Failed Back Surgery Syndrome (FBSS) at Red Butte Pain Solutions
Understanding Failed Back Surgery Syndrome (FBSS) Have you had back surgery but still feel pain? You might have what is called Failed Back Surgery Syndrome, or FBSS. This happens when back or spine surgery doesn't reduce pain or leads to new pain. At Red Butte Pain...
Back on the Greens: Rod’s Victory Over Facet Joint Pain
"Rod", is an older gentleman and an avid golfer, was one such patient. His severe back pain from facet arthritis was more than an ailment; it was a barrier between him and his passion for golf. Facet Joint Pain: A Common Adversary Facet joint pain is a widespread...
Sacroiliac Joint Pain

Sacroiliac Joint Pain: Causes, Treatment, and Relief in Arizona
Sacroiliac joint pain is a common but often misunderstood cause of lower back pain. The sacroiliac joint (SI joint) connects the sacrum, which is the base of the spine, to the pelvis. When this joint becomes irritated or inflamed, it can cause pain that radiates from the lower back to the buttocks, hips, or even the legs. For many people in Arizona, sacroiliac joint pain affects their ability to sit, walk, and perform daily activities.
Understanding the causes, symptoms, and treatments of sacroiliac joint pain is essential for finding relief.
What is the Sacroiliac Joint?
The sacroiliac joint is located where the sacrum meets the ilium bones of the pelvis. This joint has limited movement, but it plays a critical role in stabilizing the body and absorbing shock. It helps transfer the load between the upper body and the legs when walking, running, or lifting.
Due to its role in bearing weight and stabilizing the spine, the sacroiliac joint is vulnerable to stress and injury. Over time, inflammation or damage to this joint can result in significant discomfort.
Causes of Sacroiliac Joint Pain
Several factors can contribute to sacroiliac joint pain. Understanding the root cause is the first step toward effective treatment.
Injury or Trauma
A fall, car accident, or other physical trauma can damage the sacroiliac joint. Even minor injuries can result in joint inflammation, leading to chronic back pain over time.
Arthritis
Osteoarthritis can cause the sacroiliac joint’s cartilage to wear down over time. This leads to inflammation and pain in the joint. Ankylosing spondylitis, a type of inflammatory arthritis, can also affect the sacroiliac joint, causing stiffness and pain.
Repetitive Stress
Jobs or activities that involve repetitive movements, such as lifting or twisting, can stress the sacroiliac joint. Over time, this repetitive motion can lead to irritation and pain.
Leg Length Discrepancy
People with legs of different lengths may experience sacroiliac joint pain. The uneven distribution of weight causes the joint to become irritated, leading to inflammation.
Sacroiliitis
Sacroiliitis is an inflammation of the sacroiliac joint. It can be caused by arthritis, infection, or injury and often results in pain that worsens with standing or walking for long periods.
Symptoms of Sacroiliac Joint Pain
Sacroiliac joint pain often mimics other types of back pain, making it challenging to diagnose. However, there are distinct symptoms to look for:
- Lower back pain: Pain is typically felt on one side of the lower back, near the sacrum.
- Hip or buttock pain: Pain may radiate into the buttocks, hips, or thighs.
- Stiffness: The lower back may feel stiff, especially in the morning.
- Pain with movement: Pain can worsen with standing, walking, or sitting for long periods.
- Relief when lying down: Many people find that lying on their back helps relieve sacroiliac joint pain.
If you experience these symptoms, it’s essential to consult a healthcare provider to determine if the sacroiliac joint is the source of your back pain.
Diagnosing Sacroiliac Joint Pain
Diagnosing sacroiliac joint pain can be tricky because its symptoms overlap with other conditions. Your healthcare provider will likely perform a physical exam to assess your range of motion and pinpoint the pain’s location. They may also use diagnostic tests, such as:
- X-rays: To check for signs of arthritis or injury in the sacroiliac joint.
- MRI: To detect inflammation or damage to surrounding soft tissues.
- SI joint injection: A numbing injection into the sacroiliac joint can confirm if it’s the pain source. If the injection provides relief, it’s a strong indication that the SI joint is the problem.
Sacroiliac Joint Pain Treatment Options
There are various treatment options for sacroiliac joint pain, depending on the severity of the condition. A combination of treatments can help manage symptoms and improve mobility.
Physical Therapy
Physical therapy is one of the most effective treatments for sacroiliac joint pain. A physical therapist will guide you through exercises to strengthen the muscles around the sacroiliac joint and improve stability. Stretching and strengthening the muscles that support the spine and pelvis can help relieve pressure on the SI joint.
Sacroiliac Joint Injections
SI joint injections are a common treatment for sacroiliac joint pain. These injections deliver a combination of corticosteroids and anesthetic directly into the joint to reduce inflammation and relieve pain. For many patients in Arizona, sacroiliac joint injections provide significant relief from pain, allowing them to resume normal activities.
Medications
Over-the-counter pain relievers like ibuprofen and acetaminophen can help manage sacroiliac joint pain. In more severe cases, your healthcare provider may prescribe stronger anti-inflammatory medications or muscle relaxants to reduce pain and inflammation.
Chiropractic Care
Chiropractors can perform adjustments to realign the sacroiliac joint and relieve pain. Chiropractic care may be particularly helpful for people who experience sacroiliac joint dysfunction due to misalignment or repetitive stress.
Sacroiliac Joint Fusion
For severe cases of sacroiliac joint pain that don’t respond to conservative treatments, sacroiliac joint fusion may be an option. This minimally invasive surgical procedure involves fusing the bones of the sacroiliac joint to limit movement and stabilize the joint. While this procedure is more invasive, it can provide long-term relief for those suffering from chronic sacroiliac joint pain.
Lifestyle Changes to Manage Sacroiliac Joint Pain
Along with medical treatments, lifestyle changes can play a crucial role in managing sacroiliac joint pain.
Exercise and Stretching
Regular exercise and stretching can help strengthen the muscles around the sacroiliac joint. Exercises that focus on core stability, such as planks and pelvic tilts, can improve support for the spine and reduce pain. Gentle stretches that target the hips and lower back, like the piriformis stretch or hamstring stretch, can also relieve tension in the sacroiliac joint.
Posture and Body Mechanics
Maintaining good posture and using proper body mechanics can prevent further stress on the sacroiliac joint. When sitting, avoid slouching and keep your feet flat on the floor. If you must lift heavy objects, bend at your knees and use your legs to lift instead of your back.
Weight Management
Carrying excess weight can put additional pressure on the sacroiliac joint, leading to increased pain. Losing weight can help alleviate some of the stress on the joint and improve mobility.
Supportive Sleep Positions
Sleeping in a supportive position can help reduce sacroiliac joint pain. Try sleeping on your back with a pillow under your knees to keep the spine aligned. If you prefer sleeping on your side, place a pillow between your knees to reduce pressure on the hips and sacroiliac joint.
Sitting and Sleeping Comfortably with Sacroiliac Joint Pain
Finding comfortable positions for sitting and sleeping is critical when dealing with sacroiliac joint pain. Sitting for extended periods can put pressure on the SI joint and cause pain. Use the following tips to stay comfortable:
- Use a lumbar roll: A lumbar roll or cushion can support your lower back while sitting.
- Take breaks: Stand up and walk around every 30 minutes to reduce stiffness.
- Choose the right chair: Select a chair with good lumbar support and avoid soft, cushy seating that causes you to sink.
For sleeping, the following adjustments can help alleviate sacroiliac joint pain:
- Side-sleeping: Place a pillow between your knees to reduce hip and lower back strain.
- Back-sleeping: Place a pillow under your knees to maintain a neutral spine position.
Exercises to Relieve Sacroiliac Joint Pain
Exercise is crucial for relieving sacroiliac joint pain. Strengthening the muscles around the sacroiliac joint can help support the spine and reduce pain. Below are some exercises that can help:
Pelvic Tilts
-
- Lie on your back with your knees bent and feet flat on the floor.
- Tighten your abdominal muscles and tilt your pelvis upward.
- Hold for five seconds and repeat 10 times.
Bridge Exercise
-
- Lie on your back with your knees bent and feet flat on the floor.
- Lift your hips toward the ceiling, creating a straight line from your knees to your shoulders.
- Hold for five seconds and lower slowly. Repeat 10 times.
Piriformis Stretch
-
- Lie on your back with both knees bent.
- Cross one ankle over the opposite knee.
- Pull the uncrossed leg toward your chest, feeling a stretch in the buttocks.
- Hold for 20 seconds and switch legs. Repeat three times on
Find Relief from Sacroiliac Joint Pain at Red Butte Pain Solutions
If you’re struggling with sacroiliac joint pain and looking for relief, Red Butte Pain Solutions is here to help. Our team of specialists is experienced in diagnosing and treating sacroiliac joint pain, whether it’s caused by injury, arthritis, or repetitive stress. We offer personalized treatment plans that are designed to get you back to living your life without discomfort.
Don’t let sacroiliac joint pain hold you back any longer. Contact Red Butte Pain Solutions today to schedule a consultation and start your journey toward lasting relief. Whether you’re in Chandler, Tempe, Maricopa, or the surrounding Arizona area, we’re here to provide the expert care you need.
Call us at 602-633-4334 or Pre-Register to book your appointment now!
Sacroiliac Joint Exercises for Lasting Pain Relief
Sacroiliac joint (SIJ) pain is a common condition that affects the lower back and pelvis. It often results from dysfunction in the sacroiliac joints, which connect the sacrum to the iliac bones. Many individuals with SIJ pain experience discomfort when sitting,...
Are Fused Sacroiliac Joints the Answer?
The sacroiliac (SI) joints connect the spine to the pelvis, providing stability and absorbing shock. When these joints become dysfunctional due to injury, arthritis, or instability, patients can experience chronic pain in the lower back, buttocks, and legs. For some,...
The Connection Between Hip Pain and Back Pain
When I was a kid, there was a song called "The Skeleton Dance" where we sang, "The foot bone's connected to the leg bone. The leg bone's connected to the knee bone..." and so on. This simple, catchy tune shows how the body’s structures are biomechanically connected. I...
Sacroiliac Joint Pain: A Real Pain in the…
Sacroiliac (SI) joint pain can be a frustrating and debilitating condition that affects your lower back, hips, and legs. For many people in Arizona, sacroiliac joint pain interferes with daily activities, making it difficult to sit, sleep, or move comfortably. At Red...
Vertebral Compression Fractures
Vertebral Compression Fractures: Understanding Symptoms, Treatment, and Recovery
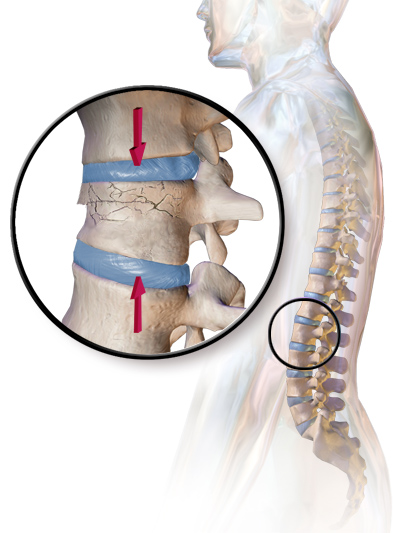
What Are Vertebral Compression Fractures?
Vertebral compression fractures (VCFs) occur when the bony block or vertebral body in the spine collapses. These fractures can lead to severe pain, deformity, and loss of height. They most commonly happen in the thoracic spine (the middle portion of the spine), especially in the lower part.
Causes of VCFs
- Osteoporosis: In people with severe osteoporosis (weak, brittle bones), VCFs may occur due to simple daily activities like stepping out of the shower, sneezing forcefully, or lifting a light object. In those with moderate osteoporosis, increased force or trauma (such as falling down or attempting to lift a heavy object) can cause a VCF.
- Age and Gender: VCFs affect an estimated 25% of all postmenopausal women in the U.S. The occurrence increases with age, affecting about 40% of women aged 80 and older. Although more common in women, VCFs are also a concern for older men.
- Trauma: People with healthy spines can suffer VCFs through severe trauma, such as car accidents, sports injuries, or hard falls.
- Metastatic Tumors: In patients younger than 55 with no history of trauma, metastatic tumors (cancer spreading to the spine) should be considered as the cause.
Symptoms of VCFs
- Sudden onset of back pain
- Increased pain intensity while standing or walking
- Decreased pain intensity while lying on the back
- Limited spinal mobility
- Eventual height loss
- Eventual deformity and disability
Seeking Medical Care
You should see a doctor to evaluate back pain if:
- You are older than 65 or younger than 12
- Your pain is the same at rest as it is while active
- You have unintentional weight loss
- You have or have had cancer
For immediate medical attention, visit an emergency department if you experience additional symptoms along with back pain.
Treatment Options
Conservative Approaches:
- Rest
- Activity modification
- Pain medication
- Limited bed rest
- Physical rehabilitation
Minimally Invasive Procedures:
- Vertebroplasty: Injecting bone cement into the fractured vertebra to stabilize it.
- Kyphoplasty: Creating space and restoring vertebral height using a balloon-like device before injecting bone cement.
Surgery:
- Surgical options include vertebroplasty, kyphoplasty, and spinal fusion surgery.
Restore Quality to Your Life
If you’re experiencing symptoms of a vertebral compression fracture, don’t wait. Contact Red Butte Pain Solutions today. Call 602-633-4334 or Pre-Register to schedule an evaluation and explore personalized treatment options. Our team of experts is here to help you find relief and improve your quality of life.
Middle Back Bone Pain: Causes and Treatment Options
Middle back bone pain can come from arthritis, fractures, or cancer. Learn what’s causing your pain and how Red Butte Pain Solutions can help.
Vertebral Compression Fracture Treatment Options for Pain Relief
Vertebral compression fractures (VCFs) affect over 700,000 Americans each year. These small spine fractures, often due to osteoporosis, trauma, or cancer, can cause intense pain and disability. Fortunately, several vertebral compression fracture treatment options can...
What Causes Aching Pain Between the Shoulder Blades?
Aching pain between the shoulder blades is a common complaint that often comes and goes. But sometimes, it can be a sign of something more serious. Understanding the potential causes can help you get the right treatment. Common Causes of Aching Pain Between the...
How Much Does A Broken Back Cost?
Over the course of my career, I've watched how the broken back cost has become a growing concern—not just for insurance companies, but for patients themselves. With rising co-pays, co-insurances, and out-of-pocket expenses, patients now bear a much larger share of the...
Managing Cancer Pain: Modern Approaches to Relief
Cancer is a life-changing diagnosis, but cancer pain does not have to control your life. Managing cancer pain is now recognized as an essential part of cancer treatment worldwide, helping patients stay active, maintain independence, and improve their quality of life....
Treatment for Broken Back Vertebra
A broken back vertebra, also known as a [vertebral compression fracture, can cause sudden, severe pain and significantly limit daily activities. These fractures are most often due to weakened bones from osteoporosis. Prompt treatment can ease pain, promote healing,...
When Back Pain Means More: Back Pain From Cancer
Back pain is common. But sometimes, it's more than a pulled muscle or a slipped disc. In some cases, back pain can be a warning sign of cancer. At Red Butte Pain Solutions, we help patients understand the cause of their pain. If you or a loved one has back pain and a...
Where Does It Hurt? Colon Cancer Pain Areas and Symptoms
Colon cancer is the second leading cause of cancer death in the United States. It often develops silently, and pain is typically a late symptom. This makes early detection and screening even more important. As the disease progresses, it can cause pain in specific...
Is a TLSO Back Brace Right for Me?
A TLSO back brace (thoracolumbosacral orthosis) is a rigid brace designed to stabilize the thoracic and lumbar spine. This provides essential support for individuals recovering from injuries, helps in managing chronic pain, and correcting postural issues. These braces...
Suffering from a Sacral Fracture? Learn Symptoms, Causes, and Treatments
As a specialized pain management practice, we frequently treat patients with sacral fractures. A sacral fracture is a break in the sacrum, the triangular bone at the base of the spine. These fractures can cause significant pain and mobility issues, affecting daily...