Kyphoplasty
Kyphoplasty: Repairing Spinal Compression Fractures
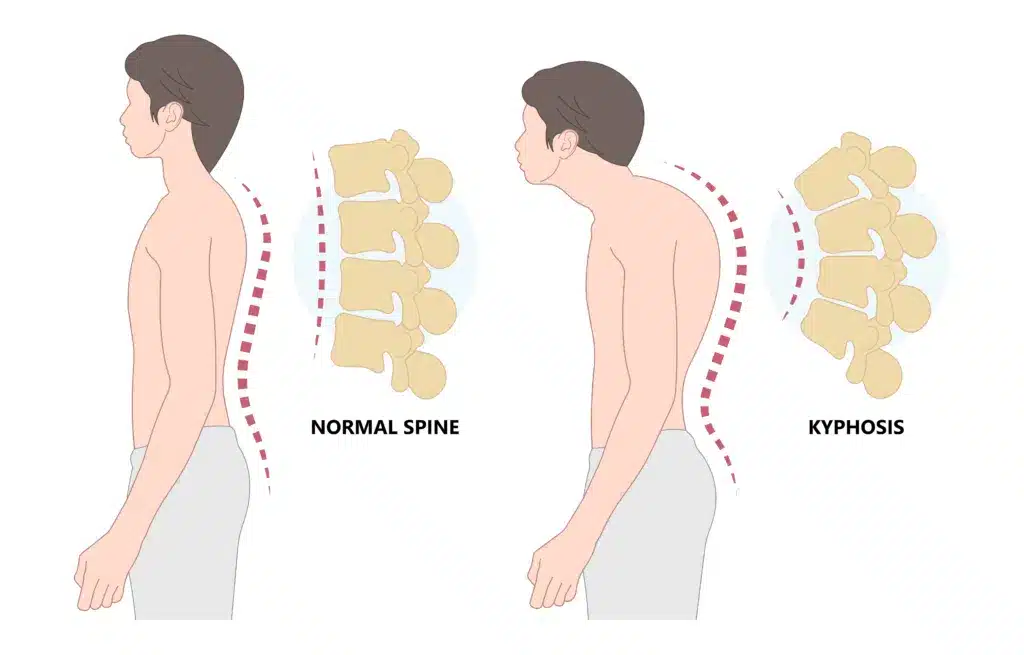
Spinal compression fractures are a common and painful condition, often caused by osteoporosis or spinal tumors. These fractures can lead to severe back pain, a “hunchback” posture known as kyphosis, reduced mobility, and a diminished quality of life. Fortunately, minimally invasive procedures like kyphoplasty and vertebroplasty offer effective treatments to stabilize the spine, relieve pain, and improve function. In this guide, we’ll explore the causes and symptoms of spinal compression fractures, explain the differences between kyphoplasty and vertebroplasty, and provide a detailed overview of these life-changing procedures.
Understanding Spinal Compression Fractures
Spinal compression fractures occur when one or more vertebrae collapse due to weakening of the bone. This condition is most often associated with osteoporosis, a disease affecting approximately 10 million Americans and placing an additional 44 million at risk. Additionally, recent data shows that more than 700,000 vertebral compression fractures are diagnosed annually in the United States. Moreover, women, particularly postmenopausal women, face a higher risk, as hormonal changes significantly impact bone density.
Symptoms of Spinal Compression Fractures
The symptoms of spinal compression fractures can vary, but they often include the following:
- Sudden, severe back pain, which is often triggered by a minor injury or strain.
- Loss of height or a noticeable curve in the spine (kyphosis).
- Difficulty standing or walking for extended periods due to spinal instability.
- Limited ability to perform daily tasks because of pain or restricted movement.
It is important to note that for many patients, conservative treatments like rest, bracing, and pain medications provide only temporary relief. However, when these measures fail to control symptoms, kyphoplasty or vertebroplasty may become the most effective options for achieving long-term pain management and spinal stability.
What Is Kyphoplasty?

Kyphoplasty is a minimally invasive surgical procedure designed to treat spinal compression fractures. The procedure involves using a small but powerful balloon to create a cavity in the broken vertebra. Once inflated, the balloon restores the vertebra’s height. Moreover, it not only stabilizes the fractured vertebra but also restores lost height, thereby helping to correct spinal alignment. Consequently, this dual benefit makes kyphoplasty particularly effective for patients experiencing significant spinal deformity or chronic pain due to compression fractures.
In addition, kyphoplasty is often performed in an office-based procedure suite, allowing patients to receive effective care without requiring a hospital stay. Furthermore, it’s an efficient option, taking only about 30 to 45 minutes per level treated.
How the Procedure Works
-
-
Preparation: To begin, the patient lies face down on a specialized table. Local anesthesia or mild sedation is administered to ensure comfort during the procedure.
-
Anesthesia and Comfort: Most kyphoplasty procedures are performed under intravenous sedation or Monitored Anesthesia Care (MAC). This type of anesthesia, similar to what patients receive during a colonoscopy, ensures both comfort and relaxation throughout the procedure.
-
Small Incisions: Next, patients typically receive one or two small incisions per level treated. These incisions are so small that they are usually closed with Dermabond, a special surgical glue, which eliminates the need for sutures or staples.
-
Balloon Insertion: Afterward, using X-ray guidance, a small tube is inserted into the fractured vertebra. A balloon catheter is then guided through the tube.
-
Cavity Creation: The balloon is carefully inflated to create a cavity within the vertebra. As a result, this restores vertebral height and reduces spinal deformity.
-
Cement Injection: Following this, the balloon is removed, and bone cement is injected into the cavity. This stabilizes the vertebra and prevents further collapse.
-
Efficient Recovery: Finally, after the procedure, patients are observed for 30 minutes in the recovery area to ensure they are stable and comfortable. Many patients experience pain relief almost immediately and are able to return to light activities within a day or two.
-
Kyphoplasty is highly regarded for its safety and effectiveness. It offers significant benefits with an exceptionally low risk of complications.
Risks and Benefits of Kyphoplasty
Kyphoplasty is highly regarded for its safety and effectiveness. Importantly, it offers significant benefits with an exceptionally low risk of complications.
Benefits of Kyphoplasty
-
- Immediate Pain Relief: Many patients report a dramatic reduction in pain within hours of the procedure. This rapid relief often improves quality of life quickly.
- Restoration of Vertebral Height: The balloon inflation not only restores the height of the fractured vertebra but also improves spinal alignment and posture.
- Improved Mobility and Function: With reduced pain and a stabilized spine, patients can comfortably return to daily activities.
- Same-Day Procedure: Additionally, the minimally invasive approach eliminates the need for an overnight hospital stay, further reducing disruption to the patient’s life.
- Minimal Scarring: Moreover, the tiny incisions used in kyphoplasty result in little to no visible scarring.
- Quick Recovery: Most patients resume light activities within a day or two, with no extended downtime required.
Risks of Kyphoplasty
While any surgical procedure carries some risk, the risks associated with kyphoplasty are remarkably low. Some potential risks include:
-
- Infection: Infection is extremely rare due to the minimally invasive technique and small incisions. The risk of infection is less than 0.1%, which is over ten times less than your risk of being in a car accident.
- Cement Leakage: Bone cement may leak outside the vertebra. However, advancements in the procedure have made this occurrence uncommon. Even when it happens, it is rarely clinically significant.
- Nerve or Soft Tissue Injury: The use of imaging guidance minimizes the risk of injury to surrounding nerves or tissues. This risk is also less than 0.1%.
- Bleeding or Hematoma: Bleeding is rare, especially in patients without a bleeding disorder.
- Allergic Reaction to Anesthesia or Materials: Allergic reactions are very uncommon, depending on individual sensitivities.
Why Choose Kyphoplasty?
Given its minimal risks and proven track record of success, kyphoplasty is a well-established option for individuals suffering from painful spinal compression fractures. Additionally, the dual benefits of stabilizing the fracture and restoring vertebral height make it a compelling choice for improving both pain and spinal alignment.
If you’re considering kyphoplasty, it’s essential to discuss your specific condition with a qualified specialist. By doing so, you can determine if this procedure is the right solution for you and take the first step toward long-term relief and recovery.
What Is Vertebroplasty?
Vertebroplasty is another minimally invasive procedure used to treat spinal compression fractures. While it shares similarities with kyphoplasty, its primary focus is on stabilizing fractures rather than restoring vertebral height. This makes vertebroplasty an effective option for patients who primarily need pain relief without significant spinal deformity.
To learn more about vertebroplasty, including detailed information about the procedure, visit our dedicated Vertebroplasty Treatment Page. There, you’ll find everything you need to understand how vertebroplasty can help reduce pain and improve your quality of life.
Kyphoplasty vs. Vertebroplasty: Key Differences
Both kyphoplasty and vertebroplasty are effective treatments for spinal compression fractures, but they serve different purposes and patient needs. Here’s a side-by-side comparison:
| Feature | Kyphoplasty | Vertebroplasty |
|---|---|---|
| Purpose | Stabilizes fractures and restores vertebral height. | Stabilizes fractures without restoring vertebral height. |
| Technique | Uses a balloon to create a cavity before cement injection. | Involves direct cement injection into the vertebra. |
| Risk of Cement Leakage | Lower due to controlled cavity creation. | Slightly higher risk of cement leakage. |
| Ideal Candidates | Patients with significant spinal deformity or chronic pain. | Patients needing pain relief for stable fractures. |
Both procedures aim to relieve pain and improve quality of life and your doctor will recommend the best option based on your specific condition.
While both kyphoplasty and vertebroplasty treat spinal compression fractures with bone cement, kyphoplasty offers an added benefit by restoring vertebral height. This makes it ideal for patients with severe compression fractures.
Choosing the Right Treatment: Kyphoplasty or Vertebroplasty?
The decision between kyphoplasty and vertebroplasty depends on various factors, including:
-
- The severity and location of the fracture.
- The presence of spinal deformity.
- Overall health and treatment goals.
Consulting with a specialist is essential to determine the best course of action for your unique needs.
When to Consider Kyphoplasty
You may be a candidate for kyphoplasty if you experience the following:
- Osteoporotic fractures in the spine causing pain or loss of height.
- Persistent back pain lasting more than four weeks, despite rest and medication.
- Vertebral compression fractures related to cancer or trauma.
- Difficulty standing upright or performing daily activities due to back pain.
- Sudden, severe back pain after minor injuries or falls.
Early treatment with kyphoplasty can prevent further spine damage and improve posture, especially for those with osteoporosis.
How Kyphoplasty Works with Bone Tumor Ablation

In addition to treating osteoporosis, kyphoplasty is often used in combination with bone tumor ablation. Bone tumor ablation treats painful spinal tumors by destroying cancerous tissue with heat or cold. Once the tumor is destroyed, kyphoplasty stabilizes the spine by reinforcing the affected vertebra with bone cement.
This combination provides effective pain relief for cancer patients and reduces the need for opioids. Moreover, it is especially helpful when the spine has become weak from metastatic cancer.
By offering this advanced treatment, Red Butte Pain Solutions helps improve quality of life for cancer patients with spinal fractures.
What to Expect During Recovery
Both kyphoplasty and vertebroplasty are outpatient procedures, meaning most patients can return home the same day. Recovery times vary, but patients typically experience:
-
- Immediate or near-immediate pain relief.
- Improved mobility and posture within a few days.
- Minimal scarring and no need for extended bed rest.
It’s important to follow your doctor’s post-procedure instructions, which may include avoiding heavy lifting and incorporating light exercises to strengthen the spine.
Tips for a Smooth Recovery:
- Avoid heavy lifting for at least two weeks.
- Stay active to prevent stiffness, but avoid strenuous activities.
- Follow your doctor’s instructions about medications and physical therapy.
- Eat calcium-rich foods and take vitamin D supplements to improve bone health.
Patients with osteoporosis should work closely with their healthcare providers to reduce the risk of future fractures.
Preventing Future Fractures
Osteoporosis is a leading cause of spinal compression fractures, and untreated osteoporosis significantly increases the risk of additional fractures. After stabilizing a fracture with kyphoplasty or vertebroplasty, it is crucial to address the underlying bone weakness to prevent future injuries.
At Red Butte Pain Solutions, we follow best practices by ensuring that every patient diagnosed with a compression fracture has a comprehensive bone health evaluation. If a patient has not had a bone density scan (DEXA scan) in the past two years, we refer them for this essential test to assess their bone density and evaluate their risk of future fractures.
Treatment Options for Osteoporosis
Most patients with osteoporosis can be safely treated with oral bisphosphonates, a class of medications that help slow bone loss and reduce fracture risk. These medications are easy to use and effective for many individuals.
However, for patients with more severe osteoporosis or those who cannot tolerate oral bisphosphonates, more advanced treatments may be necessary. We partner with local specialists, including endocrinologists and rheumatologists, to direct our patients toward the most appropriate options for their condition. These treatments may include:
- Parathyroid Hormones (e.g., Teriparatide): These medications stimulate bone growth and are highly effective for patients with severe bone loss.
- Infusion Therapy (e.g., Zoledronic Acid): Administered through an IV, these treatments offer powerful bone-strengthening effects and are often used for patients who cannot take oral medications.
Why Treating Osteoporosis Matters
Preventing future fractures is key to maintaining long-term mobility and quality of life. Spinal compression fractures can lead to chronic pain, decreased height, and spinal deformities, which can severely impact daily activities. By proactively treating osteoporosis, we reduce the likelihood of additional fractures and help our patients stay active and independent.
If you’ve experienced a spinal compression fracture, addressing your bone health is just as important as treating the fracture itself. At Red Butte Pain Solutions, we’re committed to not only relieving your pain but also helping you build a healthier, stronger future.
The Importance of Early Intervention
Untreated spinal compression fractures can lead to long-term complications, including:
- Chronic pain and reduced quality of life.
- Increased risk of additional fractures.
- Spinal deformity, such as kyphosis (hunchback).
Kyphoplasty and vertebroplasty not only provide immediate relief but also prevent further spinal damage, helping patients maintain independence and an active lifestyle.
Kyphoplasty Experts
At Red Butte Pain Solutions, we are committed to providing advanced, compassionate care to patients with back pain. Our expertise in kyphoplasty helps patients across Arizona find relief from painful spinal fractures.
We also will help direct comprehensive treatment plans for osteoporosis, including physical therapy and medication management, to help prevent future fractures. With our experience in treating cancer-related spinal fractures, we provide specialized care for those with complex needs.
Conclusion
Both kyphoplasty and vertebroplasty offer effective solutions for spinal compression fractures, helping patients regain mobility and reduce pain. By addressing the root causes of these fractures and stabilizing the spine, these procedures play a crucial role in improving quality of life.
If you or a loved one is experiencing back pain from a spinal compression fracture, don’t wait to seek treatment. Contact Red Butte Pain Solutions today at 602-633-4334 to learn more about kyphoplasty and vertebroplasty and take the first step toward a pain-free future.
Middle Back Bone Pain: Causes and Treatment Options
Middle back bone pain can come from arthritis, fractures, or cancer. Learn what’s causing your pain and how Red Butte Pain Solutions can help.
Vertebral Compression Fracture Treatment Options for Pain Relief
Vertebral compression fractures (VCFs) affect over 700,000 Americans each year. These small spine fractures, often due to osteoporosis, trauma, or cancer, can cause intense pain and disability. Fortunately, several vertebral compression fracture treatment options can...
What Causes Aching Pain Between the Shoulder Blades?
Aching pain between the shoulder blades is a common complaint that often comes and goes. But sometimes, it can be a sign of something more serious. Understanding the potential causes can help you get the right treatment. Common Causes of Aching Pain Between the...
How Much Does A Broken Back Cost?
Over the course of my career, I've watched how the broken back cost has become a growing concern—not just for insurance companies, but for patients themselves. With rising co-pays, co-insurances, and out-of-pocket expenses, patients now bear a much larger share of the...
Managing Cancer Pain: Modern Approaches to Relief
Cancer is a life-changing diagnosis, but cancer pain does not have to control your life. Managing cancer pain is now recognized as an essential part of cancer treatment worldwide, helping patients stay active, maintain independence, and improve their quality of life....
Treatment for Broken Back Vertebra
A broken back vertebra, also known as a [vertebral compression fracture, can cause sudden, severe pain and significantly limit daily activities. These fractures are most often due to weakened bones from osteoporosis. Prompt treatment can ease pain, promote healing,...
Where Does It Hurt? Colon Cancer Pain Areas and Symptoms
Colon cancer is the second leading cause of cancer death in the United States. It often develops silently, and pain is typically a late symptom. This makes early detection and screening even more important. As the disease progresses, it can cause pain in specific...
Aching Mid Back Pain After a Car Accident – Am I Totalled?
Car accidents can lead to a variety of injuries, even when the collision seems minor. Recently, I treated a patient who experienced aching mid-back pain after being rear-ended by a Tesla. Despite Teslas appearing small, their electric batteries make them significantly...
Can Prostate Cancer Cause Back Pain?
As a pain management physician, I often hear the question, “Doc, can prostate cancer cause back pain?” The short answer is yes, prostate cancer can cause back pain. However, it’s crucial to understand that back pain has many causes, and most of the time, the...
Osteoporosis Explained: Symptoms, Screening, and Treatment
At Red Butte Pain Solutions, we frequently see patients struggling with osteoporosis symptoms. Many of these patients come to us because of painful vertebral compression fractures. These fractures often result from weakened bones caused by osteoporosis, making it a...