Nerve pain in cancer—also known as neuropathic cancer pain (NCP)—is a complex and often debilitating type of pain. It affects a significant number of patients either due to direct tumor invasion or as a side effect of cancer treatments like surgery, chemotherapy, or radiation.
Unlike nociceptive pain, which results from tissue injury, NCP stems from nerve damage. This type of pain is often persistent, resistant to standard treatments, and emotionally distressing for patients and their families.

What Causes Nerve Pain in Cancer?
Nerve pain in cancer may stem from several mechanisms:
- Tumor Infiltration: Tumors may directly compress or invade peripheral or central nerves, causing irritation and inflammation. This often results in sharp, burning, or electric-like sensations.
- Surgery: Surgical procedures to remove tumors or lymph nodes may unintentionally damage nearby nerves. Postsurgical nerve pain can persist for months or years.
- Chemotherapy: Up to 90% of patients receiving neurotoxic chemotherapy drugs, such as taxanes and platinum agents, develop chemotherapy-induced peripheral neuropathy (CIPN).
- Radiation Therapy: Radiation can lead to delayed nerve damage, particularly in the brachial or lumbosacral plexus, resulting in progressive neuropathic symptoms.
Symptoms of Nerve Pain in Cancer
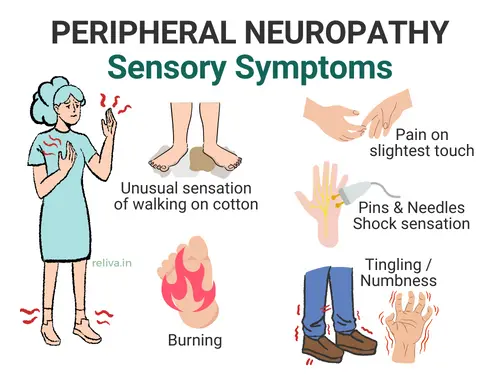
Patients with NCP may experience a broad range of symptoms, including:
- Tingling, burning, or stabbing sensations in hands, feet, or affected areas
- Numbness or hypersensitivity to touch or temperature
- Muscle weakness or altered gait
- Pain that intensifies at night or with even light pressure (allodynia)
These symptoms can significantly interfere with sleep, mobility, and overall quality of life.
No Proven Way to Prevent It—Yet
As of now, there is no definitive preventive strategy for NCP. According to ASCO guidelines, no medications or supplements have consistently demonstrated efficacy in preventing neuropathic pain related to cancer. However, early screening and frequent reassessment in high-risk patients can help detect emerging neuropathy and prompt early interventions that may prevent progression.
Pre-Existing Neuropathy and Cancer Treatment
Patients with pre-existing neuropathy—such as painful diabetic peripheral neuropathy (DPN)—are at significantly higher risk of worsening symptoms during cancer treatment. Studies show that diabetes is an independent risk factor for developing more severe CIPN, with odds ratios ranging from 1.60 to 2.17.
Neurotoxic chemotherapy agents like paclitaxel, cisplatin, and vincristine can be particularly harmful to these patients. The presence of DPN amplifies the neurotoxic effects, often resulting in dose reductions, treatment interruptions, or persistent neuropathic pain.
A thorough pre-treatment assessment is vital. This includes evaluating neuropathy severity, pain levels, mobility, sleep, mood disorders, and potential drug interactions. First-line medications such as gabapentin, pregabalin, and duloxetine are effective in managing both DPN and NCP. Tricyclic antidepressants and topical agents like lidocaine and capsaicin patches may provide additional relief.
Non-drug strategies are important adjuncts. Physical therapy, aerobic exercise, and transcutaneous electrical nerve stimulation (TENS) can help restore function and reduce pain. For refractory DPN, 10-kHz spinal cord stimulation (SCS) has strong evidence for improving pain and function. In cancer-related cases, interventional procedures like epidural infusions and nerve blocks may be considered.
Early intervention and close monitoring are essential. Oncologists, endocrinologists, and pain specialists must collaborate closely to tailor regimens that minimize harm while optimizing pain control and treatment efficacy.
Treatment Options for Nerve Pain in Cancer
Managing NCP effectively requires a multidisciplinary and multimodal approach. The following treatments are commonly used:
Pharmacologic Treatments
- Opioids: Often used for moderate to severe cancer pain. However, they are generally less effective for neuropathic pain due to differences in how nociceptive and neuropathic pain are processed in the nervous system.
- Adjuvant Analgesics:
- Anticonvulsants: Gabapentin and pregabalin modulate calcium channels to reduce nerve excitability.
- Antidepressants: Duloxetine (an SNRI) and tricyclics like amitriptyline block pain pathways via serotonin and norepinephrine.
- Topicals: Lidocaine patches or capsaicin 8% patches offer relief for localized pain.
- Corticosteroids: Often used for radiculopathy or compression-related inflammation, particularly in cases involving vertebral body compression fractures.
ASCO specifically recommends duloxetine for treating painful CIPN, making it a cornerstone pharmacologic option.
Non-Pharmacologic Therapies
- Physical Therapy and Rehabilitation: Structured rehab programs can improve strength, flexibility, and function.
- Oncologic Management: Reducing tumor size with radiation, surgery, or chemotherapy can sometimes alleviate the underlying source of pain.
- Exercise: Moderate aerobic and resistance training is safe during cancer treatment and can reduce CIPN severity.
- Acupuncture and Scrambler Therapy: These non-invasive therapies have shown promise in reducing chronic neuropathic symptoms and improving quality of life.
Nutritional and Experimental Options
Some dietary supplements and nutraceuticals are under investigation for neuropathic pain, though guidelines remain cautious:
- Alpha-Lipoic Acid (ALA): A potent antioxidant used for diabetic neuropathy. Results are mixed for CIPN, with some benefit in breast cancer trials but negative findings in platinum-based regimens.
- Glutamine: Proposed to reduce neuroinflammation. Limited studies show inconsistent benefit.
- Omega-3 Fatty Acids: Their anti-inflammatory properties may help prevent or reduce CIPN, though larger trials are needed.
- Vitamin B Complex and Vitamin E: B6 and B12 have potential neuroprotective effects. Vitamin E use is limited due to possible cancer risk.
- Melatonin, N-acetylcysteine (NAC), and other phytochemicals: Show promise in animal models but require more human data.
Avoid: Acetyl-L-carnitine, which may worsen symptoms of CIPN.
Duloxetine and Lidocaine Infusions for Prevention
Emerging research suggests that early use of duloxetine or lidocaine infusions may reduce the likelihood and severity of taxane-induced peripheral neuropathy. One randomized controlled trial found that both interventions significantly lowered neuropathy severity and improved patient-reported outcomes in high-risk breast cancer patients.
Duloxetine, a serotonin-norepinephrine reuptake inhibitor (SNRI), works by increasing levels of norepinephrine and serotonin in the central nervous system. These neurotransmitters modulate descending pain inhibition pathways and help reduce both central and peripheral sensitization. Additionally, duloxetine influences the neuroendocrine stress axis, enhancing its analgesic effects in patients with neuropathic pain.
Clinical trials have demonstrated that duloxetine significantly reduces chemotherapy-induced neuropathic pain, particularly from agents like taxanes and platinum compounds. Patients report meaningful improvements in both symptom intensity and quality of life. It is the only pharmacologic agent recommended by the American Society of Clinical Oncology (ASCO) for established painful CIPN.
Lidocaine, a sodium channel blocker, works by inhibiting the abnormal electrical discharges in damaged nerves. It reduces peripheral nerve excitability and central hyperexcitability, both of which contribute to chronic neuropathic pain. Lidocaine also affects NMDA receptor activity and may help prevent central sensitization.
A randomized controlled study comparing lidocaine infusions to duloxetine in breast cancer patients receiving taxane chemotherapy found that both treatments were equally effective in preventing neuropathy. Lidocaine infusions resulted in both immediate pain relief and moderate long-term reduction in symptoms. In many patients, the benefits of a single infusion lasted up to three weeks, though repeat dosing schedules may be needed for sustained relief.
These options may be especially helpful in patients with a history of neuropathy or those receiving aggressive combination chemotherapy.
Glutamate’s Emerging Role in Nerve Pain
Glutamate is an excitatory neurotransmitter involved in pain signaling. In cancer, tumor cells can release excess glutamate via system xc-, leading to increased nociceptive input and sensitization.
Preclinical studies have shown that inhibiting this glutamate transporter (e.g., with sulfasalazine) reduces cancer-induced bone pain. While not yet clinically validated, glutamate-modulating therapies offer a novel direction for future research and potential treatment of NCP.
Final Thoughts
Nerve pain in cancer is more than a physical burden—it can disrupt every part of a patient’s life. From sleep and walking to coping with treatment and holding onto hope, neuropathic pain creates deep and lasting challenges.
However, with early assessment, personalized care, and collaboration across specialties, nerve pain in cancer can be effectively managed. Every patient deserves relief, dignity, and a treatment plan built around their unique needs and goals.
If you’re living with nerve pain from cancer or its treatments, Red Butte Pain Solutions provides compassionate, evidence-based care tailored just for you.
📞 Call us at 602-633-4334
🔗 Schedule now to take the first step toward relief.
We welcome patients from Chandler, Ahwatukee, Laveen, Sun Lakes, Casa Grande, Maricopa, Gilbert, Mesa, Tempe, and South Phoenix.
