Lumbar Facet Arthropathy
Introduction
Related Topics:
Facet arthropathy is a leading cause of chronic back pain. Impacting an estimated 30-40% of individuals with chronic lower back pain worldwide. This degenerative condition develops when the small joints in the spine, called facet joints, wear down. This leads to inflammation, pain, and restricted movement. Over time, untreated facet arthropathy can significantly impact mobility and quality of life. At Red Butte Pain Solutions, we specialize in advanced pain management solutions for facet arthropathy. If you’re struggling with persistent back pain, understanding the condition’s causes, symptoms, and treatment options is essential. This guide provides a comprehensive overview of facet arthropathy and how to manage it effectively.
What is Facet Arthropathy?
Facet arthropathy refers to the degenerative changes that occur within the facet joints of the spine.
What Do Facet Joints Do?
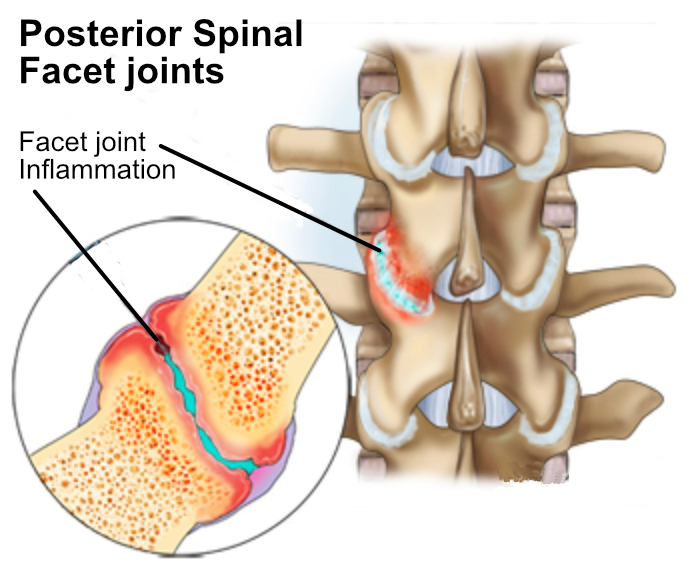
These small stabilizing joints provide support and allow for controlled spinal movements, such as bending, twisting, and arching. They work in coordination with intervertebral discs to maintain spinal stability while enabling flexibility. The facet joints help guide motion while the discs act as shock absorbers, preventing excessive movement and distributing loads evenly across the spine. When facet joints deteriorate, this balance is disrupted, increasing stress on the discs and nearby structures. This can speed up degeneration and worsen pain. When the protective cartilage within these joints erodes, the bones begin to rub against each other, triggering pain, swelling, and stiffness.
Where Do We Most Often Get This?
Facet arthropathy most commonly affects the cervical (neck) and lumbar (lower back) regions because these areas bear the most movement and weight. The thoracic spine is less affected because the ribcage supports it. This limits movement and reduces stress on facet joints. The lumbar spine supports the upper body and absorbs impact from activities like walking and lifting, while the cervical spine enables head and neck motion, making both regions prone to wear and tear.
Experiencing Facet Joint Pain
While some individuals experience only localized pain, others may develop radiating discomfort that extends to the shoulders, buttocks, or legs. Facet joint pain is typically described as an aching or dull pain that worsens with prolonged standing, bending, or twisting. Unlike nerve-related pain such as sciatica, which often follows a distinct nerve pathway and may be accompanied by numbness, tingling, or weakness, facet joint pain is more diffuse and localized to the affected joint region. Distinguishing between these types of pain is essential for determining the most effective treatment approach. The severity of symptoms depends on the stage of degeneration. The following stages outline how symptoms progress, from mild discomfort to severe mobility restrictions, helping to determine the most appropriate treatment approach.
Stages of Lumbar Facet Arthropathy
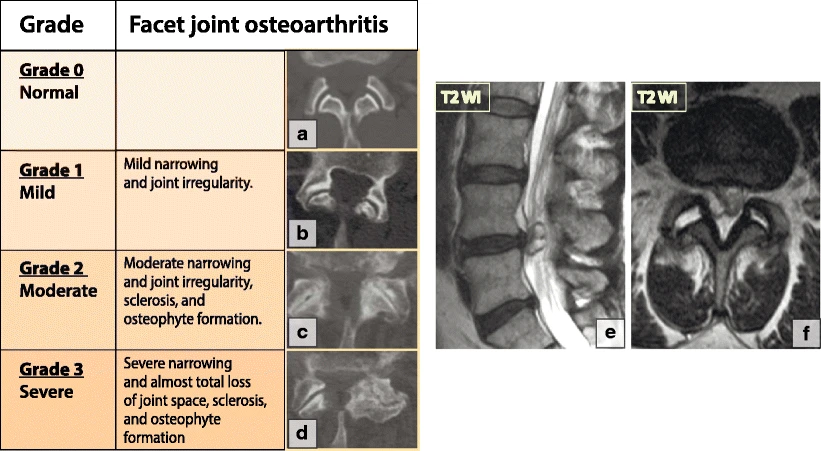
Facet arthropathy progresses gradually through four key stages, each representing an increasing level of joint degeneration and associated symptoms. Recognizing these stages is important for determining the most effective treatment strategies. Early intervention can help slow progression, while advanced stages may require more aggressive treatments to manage pain and mobility issues.
Early Degeneration: Cartilage within the facet joints begins to thin, leading to minor inflammation. Pain may be intermittent and occur primarily after prolonged activity or specific movements.
Moderate Degeneration: Increased cartilage loss leads to the development of bone spurs, which can cause stiffness and more persistent pain, particularly in the morning or after periods of inactivity.
Severe Degeneration: At this stage, significant cartilage loss results in bone-on-bone contact. Pain becomes chronic, movement is noticeably restricted, and joint instability may develop.
Advanced Facet Arthropathy: Facet joint enlargement (hypertrophy) may occur, compressing nearby nerves and potentially leading to spinal stenosis. Pain is severe, mobility is greatly impaired, and nerve-related symptoms such as numbness or tingling may appear.
Causes of Facet Arthropathy
Several factors contribute to the development of facet arthropathy:
-
-
Aging: The natural aging process leads to cartilage deterioration, increasing the risk of arthritis.
-
Repetitive Stress: Repetitive spinal movements, such as bending, lifting, and twisting, accelerate joint wear and tear.
-
Spinal Injury: Traumatic events, including car accidents, falls, and sports-related impacts, can damage facet joints, leading to early degeneration. Direct trauma may cause fractures, dislocations, or excessive joint stress, resulting in cartilage breakdown and inflammation. Even minor injuries, such as whiplash, can accelerate facet joint degeneration over time. Additionally, repetitive microtrauma from activities that place excessive strain on the spine, like heavy lifting or contact sports, can contribute to gradual joint deterioration and the onset of facet arthropathy.
-
Spinal Misalignment: Conditions like scoliosis or spondylolisthesis put uneven pressure on the facet joints, contributing to cartilage breakdown.
-
Obesity: Excess weight increases strain on the lower back, speeding up degenerative changes.
-
Previous Spinal Surgery: Changes in spinal mechanics following surgery can place excessive stress on the facet joints, leading to arthropathy.
-
Symptoms of Facet Arthropathy
The symptoms of facet arthropathy vary depending on the severity and location of joint degeneration. Common symptoms include:
-
-
Localized Back Pain: Persistent aching pain in the affected region, often worsening with movement.
-
Stiffness: Reduced spinal flexibility, particularly in the morning or after prolonged sitting.
-
Pain with Movement: Activities such as bending, twisting, or arching the back can intensify discomfort.
-
Radiating Pain: Pain may extend to the buttocks, thighs, shoulders, or upper arms depending on the affected area.
-
Muscle Spasms: The muscles surrounding the spine may tighten in response to joint instability, exacerbating pain.
-
Reduced Range of Motion: As degeneration progresses, movements become more restricted, impacting daily activities.
-
Lumbar Facet Joint Pain Referral Patterns
Lumbar facet arthropathy often presents with characteristic pain referral patterns. Pain from the upper lumbar facet joints (L1-L3) typically refers to the flank, hip, or groin region, sometimes mimicking hip pathology. Mid-lumbar facet joints (L3-L4) often cause pain radiating into the lateral thigh. Lower lumbar facet joints (L4-L5 and L5-S1) frequently refer pain to the buttocks and posterior thighs, sometimes resembling sciatica but without true nerve compression. Recognizing these referral patterns helps distinguish facet joint pain from other conditions like disc herniation or radiculopathy.

Diagnosing Facet Arthropathy
At Red Butte Pain Solutions, we use a multi-step diagnostic approach:
-
-
Medical History: A thorough evaluation of symptoms, past injuries, and medical conditions.
-
Physical Examination: Assessing spinal flexibility, range of motion, and areas of tenderness.
-
Imaging Tests: X-rays, MRI scans, or CT scans help visualize joint space narrowing, cartilage loss, and bone spur formation.
-
Diagnostic Injections: A local anesthetic injection into the facet joint can confirm the source of pain if relief follows the procedure.
-
Treatment Options for Facet Arthropathy
Related Topics:
Managing facet arthropathy involves a combination of conservative, interventional, and surgical treatments.
Conservative Management
Physical Therapy
Strengthens spinal-supporting muscles, improves flexibility, and enhances posture.
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can help reduce inflammation and relieve pain. Acetaminophen may be recommended for individuals who cannot tolerate NSAIDs. In more severe cases, prescription medications like muscle relaxants, nerve pain medications (such as gabapentin or pregabalin), or low-dose antidepressants may be used to manage chronic pain. For short-term relief, corticosteroids or opioid medications may be prescribed, but these are typically reserved for cases where other treatments have been ineffective due to potential risks and side effects.
Heat and Cold Therapy
Alternating heat and ice therapy can help alleviate stiffness, inflammation, and muscle tension associated with facet arthropathy. Applying heat relaxes tight muscles, increases blood circulation, and improves joint flexibility, making it particularly beneficial before physical activity. Cold therapy, on the other hand, helps numb pain, reduce swelling, and minimize inflammation after activity or injury. Patients can use heating pads, warm baths, or ice packs for relief, ensuring they follow proper application techniques to avoid skin damage.
Lifestyle Modifications
Maintaining a healthy weight, practicing proper posture, and avoiding repetitive spinal strain are key to managing facet arthropathy and preventing further degeneration. Engaging in regular low-impact exercises, such as swimming or walking, helps strengthen the muscles that support the spine, reducing stress on the facet joints. Additionally, ergonomic adjustments, such as using lumbar support while sitting and sleeping on a supportive mattress, can help maintain proper spinal alignment. Avoiding prolonged sitting or standing and incorporating movement throughout the day can further alleviate strain on the back.
Interventional Pain Management
When conservative methods do not provide sufficient relief, interventional treatments may be necessary:
-
- Facet Joint Injections: Injecting corticosteroids and anesthetics directly into the facet joint to reduce inflammation and provide temporary pain relief.
- Radiofrequency Ablation (RFA): A minimally invasive procedure that disrupts pain signals by applying heat to the affected nerve endings. This technique targets the medial branch nerves that transmit pain from the facet joints, effectively blocking pain signals. RFA offers long-lasting pain relief, typically for six months to a year, though some patients experience relief for even longer. The procedure is performed under fluoroscopic guidance to ensure precise nerve targeting and involves a short recovery time, allowing most patients to resume normal activities within a few days.
Surgical Options
Surgery is considered only when all other treatments have failed and the patient experiences severe, persistent pain, significant loss of mobility, or nerve compression leading to weakness or numbness. The decision for surgery is typically based on imaging findings, response to previous treatments, and the overall impact on daily life.
Facet Joint Replacement
A newer surgical option that involves replacing the damaged facet joint with an artificial implant. This procedure aims to preserve spinal motion while alleviating pain and reducing joint degeneration. It is considered for select patients who may not require fusion but need structural joint support.
Facet Joint Fusion
A surgical procedure that permanently fuses two or more vertebrae to eliminate movement in the affected joint and stabilize the spine. This procedure is typically recommended for patients with severe facet arthropathy who experience chronic pain and instability that does not respond to conservative or interventional treatments. The surgery involves the use of bone grafts, metal rods, and screws to facilitate the fusion process. Over time, the vertebrae grow together, reducing painful motion and preventing further degeneration. While recovery can take several months, physical therapy and rehabilitation play a crucial role in regaining strength and mobility post-surgery.
Laminectomy
A surgical approach that removes part of the vertebra, specifically the lamina, to relieve nerve compression in cases of advanced facet arthropathy and spinal stenosis. This procedure creates more space within the spinal canal, reducing pressure on the spinal cord and nerve roots. It is often recommended when patients experience severe pain, weakness, or numbness that does not improve with conservative treatments. Depending on the severity of the condition, laminectomy may be performed alone or in combination with other procedures, such as spinal fusion, to provide additional stability. Recovery involves physical therapy to restore mobility and strengthen the muscles supporting the spine.
Preventing Facet Arthropathy
While facet arthropathy cannot always be prevented, these strategies can help reduce risk and slow progression:
-
-
Vitamins and Supplements: Incorporating supplements such as vitamin D, calcium, and omega-3 fatty acids may support bone and joint health, potentially slowing the progression of facet arthropathy. Glucosamine and chondroitin are also commonly used to promote cartilage integrity and reduce inflammation.
-
Weight Management: Reducing excess weight lessens spinal strain and joint pressure.
-
Regular Exercise: Engaging in low-impact activities like swimming, walking, or yoga strengthens the spine, maintains flexibility, and improves overall spinal health. These exercises help stabilize the core muscles, reduce stress on the facet joints, and enhance posture. Strength training focused on the back and abdominal muscles can further support the spine, minimizing the impact on affected joints. Additionally, incorporating balance exercises, such as tai chi or Pilates, can help improve coordination and reduce the risk of falls, which can worsen spinal conditions. Regular movement prevents stiffness and enhances blood circulation to the joints, promoting healing and reducing inflammation associated with facet arthropathy.
-
Ergonomic Support: Using supportive chairs, proper mattress alignment, and maintaining good posture minimizes stress on the spine.
-
Stretching Routines: Incorporating daily stretches helps prevent stiffness and promotes spinal mobility.
-
Dealing With Your Facet Arthropathy
Facet arthropathy is a progressive condition that can significantly impact daily life. Managing it effectively requires understanding its stages, symptoms, and available treatments. By adopting lifestyle changes, engaging in targeted therapies, and seeking professional care, individuals can reduce pain and improve mobility. Early intervention and personalized treatment plans play a crucial role in preventing further degeneration and maintaining spinal health. Understanding its stages, symptoms, and treatment options is crucial for effective management. At Red Butte Pain Solutions, we provide personalized treatment plans to help patients find relief from facet arthropathy in Arizona. Whether you’re seeking conservative care, interventional procedures, or advanced pain management strategies, we are here to support you.
If you’re struggling with persistent back pain, contact Red Butte Pain Solutions at 602-633-4334 to schedule a consultation and start your journey toward lasting relief.
What Causes Aching Pain Between the Shoulder Blades?
Aching pain between the shoulder blades is a common complaint that often comes and goes. But sometimes, it can be a sign of something more serious. Understanding the potential causes can help you get the right treatment. Common Causes of Aching Pain Between the...
The Connection Between Hip Pain and Back Pain
When I was a kid, there was a song called "The Skeleton Dance" where we sang, "The foot bone's connected to the leg bone. The leg bone's connected to the knee bone..." and so on. This simple, catchy tune shows how the body’s structures are biomechanically connected. I...
Radiofrequency Ablation: Relief for Chronic Pain
At Red Butte Pain Solutions, radiofrequency ablation (RFA) is one of our most effective tools for treating chronic pain. This minimally invasive procedure uses heat generated by radio waves to target specific nerves and disrupt their ability to transmit pain signals....
Back Pain: Finding Causes and Effective Back Pain Relief
Back pain is a common issue that affects millions of people each year. Back pain can range from mild discomfort to severe, chronic pain that disrupts daily life. While simple remedies like stretching or massage offer relief for many, these solutions may only provide...
Failed Back Surgery Syndrome (FBSS) at Red Butte Pain Solutions
Understanding Failed Back Surgery Syndrome (FBSS) Have you had back surgery but still feel pain? You might have what is called Failed Back Surgery Syndrome, or FBSS. This happens when back or spine surgery doesn't reduce pain or leads to new pain. At Red Butte Pain...
Back on the Greens: Rod’s Victory Over Facet Joint Pain
"Rod", is an older gentleman and an avid golfer, was one such patient. His severe back pain from facet arthritis was more than an ailment; it was a barrier between him and his passion for golf. Facet Joint Pain: A Common Adversary Facet joint pain is a widespread...
