
“Is diabetic nerve pain reversible?” This is one of the most common questions I hear from patients at Red Butte Pain Solutions. Diabetic peripheral neuropathy (DPN) can be frustrating and life-changing, especially when patients feel like their symptoms are progressing despite their best efforts. Let’s break down what the science says and explore the treatment options that are available.
Understanding Diabetic Peripheral Neuropathy
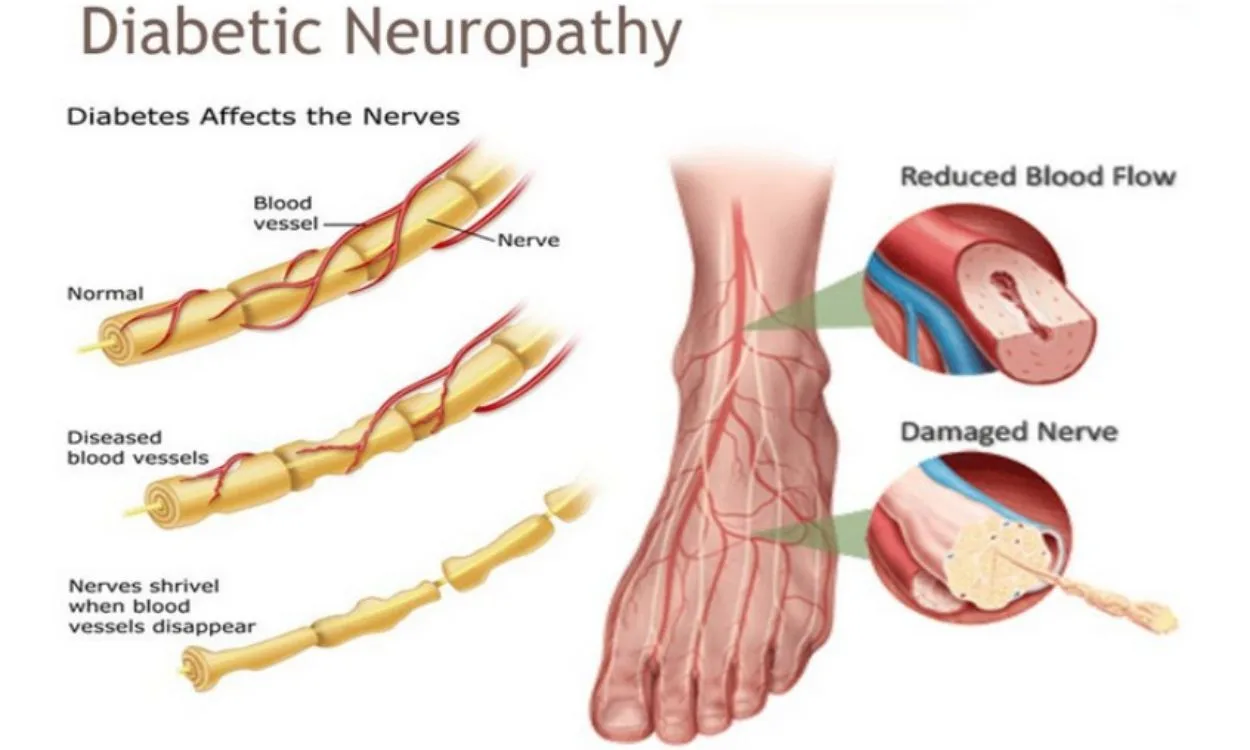
Diabetic peripheral neuropathy is nerve damage caused by diabetes, typically affecting the legs and feet. Symptoms include burning, tingling, numbness, and stabbing pain. Over time, this condition can lead to significant sensory loss, increasing the risk of foot injuries and ulcers.
Can It Be Reversed?
So, “is diabetic nerve pain reversible?” Unfortunately, the answer is almost always no. Once nerve damage from diabetic neuropathy is established, there are no current treatments that can reliably reverse it.
Even when pain is better controlled, the loss of sensation that places patients at risk for injury, ulceration, and infection generally persists. As such, while patients may feel better, their nerves remain damaged.
Pharmacologic agents like gabapentinoids, SNRIs, tricyclic antidepressants, sodium channel blockers, and topical therapies may reduce pain. However, they do not restore lost nerve function or sensation. These treatments work by altering how pain signals are transmitted or perceived in the brain and spinal cord—not by healing or regenerating the damaged nerves themselves. They modulate neurotransmitters, block sodium or calcium channels, or affect reuptake pathways, offering symptomatic relief without addressing the underlying structural damage.
How Loss of Sensation Leads to Ulcers and Amputation
When sensation is lost, the body loses its early warning system. A person with DPN might not feel a rock in their shoe or a blister forming. Without the pain signal that would normally prompt someone to address an injury, that small wound can worsen. Friction or pressure continues to damage the skin until an ulcer forms—often at high-pressure points like the heel, ball of the foot, or toes.
If an ulcer becomes infected, the situation can escalate quickly. Infections in people with diabetes are often harder to control, and reduced blood flow makes healing more difficult. What started as a minor issue can spiral into a serious complication requiring hospitalization—or even lead to amputation.
This is why preserving or restoring protective sensation in the feet is so important. It’s not just about comfort—it’s about safety, mobility, and quality of life.
Glycemic Control: Helpful, But Not Reversing
Tight blood sugar control can slow the progression of diabetic neuropathy, especially in patients with type 1 diabetes. However, even intensive glycemic management does not typically restore nerve function once the damage is done.
Lifestyle Modifications That Help
While reversal may not be possible, certain lifestyle changes can play a critical role in slowing disease progression and preserving function. These include:
- Quitting smoking
- Losing excess weight
- Managing blood pressure and cholesterol
- Staying physically active
- Eating a nutrient-rich, anti-inflammatory diet
These efforts reduce vascular stress, inflammation, and oxidative injury to nerves. Addressing these risk factors may not reverse nerve damage but can help prevent it from worsening. To learn more, visit our post on risk factors for painful diabetic neuropathy.
A Glimmer of Hope with Spinal Cord Stimulation
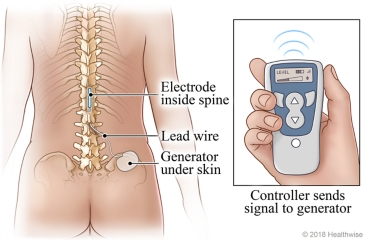
Emerging research on high-frequency spinal cord stimulation (HFX, 10 kHz) offers some promising outcomes. While it does not reverse neuropathy in the traditional sense, it has shown the potential to improve protective sensation in the feet.
In randomized trials such as the SENZA-PDN study, patients treated with HFX stimulation experienced increased numbers of sensate locations during 10-gram monofilament testing. These improvements were not just statistical—they were clinically meaningful. Patients who previously could not feel certain areas of their feet regained enough sensation to be reclassified from high-risk to low-risk for foot ulcers.
These changes were sustained over 24 months and accompanied by reductions in foot ulcer risk, infection, and even potential amputation. Improving sensation may reduce morbidity and mortality by preventing complications that often begin with a numb, injured foot that goes unnoticed until it’s too late.
One particularly striking finding is that up to 65% of patients demonstrated neurological improvement at long-term follow-up. Histological studies even suggest increases in intra-epidermal nerve fiber density, which raises the possibility of actual nerve regeneration.
While the exact mechanism remains unclear, researchers have proposed theories such as stochastic resonance, where consistent neuromodulation helps amplify weak sensory signals in the damaged nervous system, making them more perceptible.
Regardless of mechanism, the results speak for themselves—patients are gaining back function, not just pain control. Restoring sensation can reduce the risk of infections and amputations and, in many cases, can even save lives.
We offer HFX spinal cord stimulation at Red Butte Pain Solutions as part of our advanced approach to treating DPN.
How DPN Affects Daily Life
Living with diabetic peripheral neuropathy can impact almost every aspect of daily life. Many patients have trouble walking due to pain, numbness, or instability. Even simple tasks like shopping or cleaning can become exhausting. Driving can feel unsafe when sensation in the feet is impaired.
The emotional toll is just as significant. Constant pain and fear of complications can lead to anxiety, depression, and isolation. Sleep quality may suffer, work performance may decline, and hobbies may be abandoned.
The good news is that even though we can’t reverse DPN, we can help you take control of your life again—with pain relief, mobility support, and tools to prevent complications.

What This Means for You
If you are living with diabetic nerve pain, it’s understandable to hope for a cure. While true reversal is unlikely, there are many treatments that can reduce pain, improve function, and potentially slow progression.
One of the most exciting developments in recent years is high frequency spinal cord stimulation.
To learn whether this therapy could help you—or to explore other options for painful diabetic neuropathy—schedule now or call us at 602-633-4334.
Final Thoughts
Though diabetic nerve pain is not reversible with current treatments, you are not powerless. Our team is here to help you reduce pain, preserve function, and stay active.
We proudly serve patients from Mesa, Chandler, Gilbert, Tempe, Ahwatukee, Sun Lakes, Maricopa, Laveen, and Casa Grande.
