
Cancer pain can be relentless. For many, it disrupts daily life, interferes with sleep, and saps the will to keep fighting. Thankfully, there is hope for cancer pain relief. At Red Butte Pain Solutions, we specialize in offering tailored, effective treatments that restore dignity and comfort.
Whether you’re newly diagnosed, undergoing treatment, or in recovery, there are options for meaningful cancer pain relief.
Why Cancer Pain Is So Common—and So Important to Treat
- 59% of patients receiving active cancer treatment
- 64% of patients with advanced cancer
- 33% of cancer survivors, even after curative treatment

Clearly, unmanaged pain lowers quality of life, limits function, and worsens emotional health. On top of that, studies suggest that timely pain management may even improve survival.
Unfortunately, cancer pain often goes undertreated. As a result, many patients with severe pain do not receive the medications they truly need for relief.
The “5 A’s” of Cancer Pain Relief
- Analgesia – Pain control
- Activities – Maintaining independence
- Adverse Effects – Minimizing side effects
- Aberrant Behaviors – Monitoring misuse
- Affect – Supporting emotional wellness
Importantly, this approach requires a multidisciplinary team: cancer doctors, nurses, pain specialists, physical therapists, and counselors all contribute meaningfully.
Step One: Comprehensive Pain Assessment
To treat pain effectively, we must first understand it. Cancer pain may be:
- Nociceptive – from tumors pressing on tissues or bones
- Neuropathic – from nerve injury or chemotherapy
- Mixed – a combination of both
Accordingly, clinicians use validated pain scales, evaluate functional impact, and reassess regularly to ensure proper treatment response.
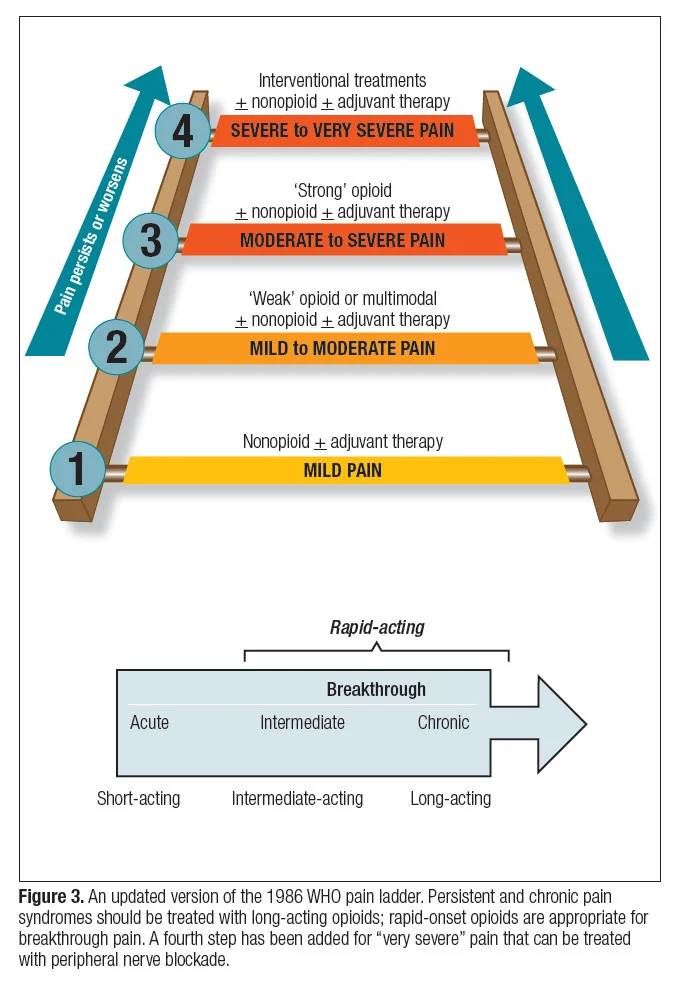
Step Two: The WHO Pain Ladder
The World Health Organization (WHO) recommends a stepwise approach to medications. Though widely recognized, the ladder’s second step is often bypassed.
Non-Opioid Medications
- Acetaminophen, ibuprofen, or naproxen
- Work best for mild pain, especially when associated with bone involvement
Weak Opioids
- Codeine, tramadol
- Sometimes skipped due to limited efficacy
Strong Opioids
- Morphine, oxycodone, fentanyl, methadone
- Often prescribed in a combination of long-acting and short-acting formulations
Adjuvant Medications
- Antidepressants, anticonvulsants, corticosteroids
- These are especially helpful for nerve pain and targeted syndromes
Step Three: Managing Side Effects and Safety
Opioids are effective but come with side effects like constipation, nausea, and fatigue. Fortunately, most side effects can be proactively managed.
Additionally, providers routinely monitor for misuse using:
- Prescription drug monitoring programs
- Urine drug testing when appropriate
- Structured risk assessments
When no longer required, opioids should be safely tapered with supervision.
Intrathecal Drug Delivery: When Standard Treatments Aren’t Enough
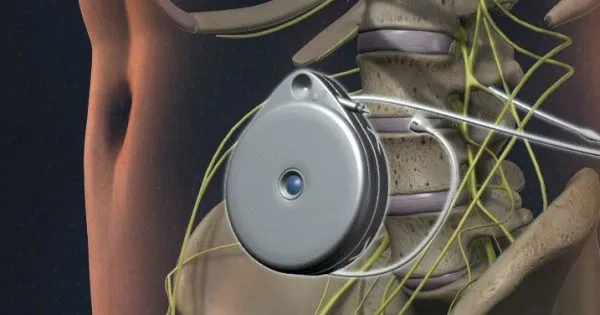
For some, stronger, more targeted relief becomes necessary. That’s where intrathecal drug delivery systems (IDDS) — also known as pain pumps — offer an advanced solution.
What Are Intrathecal Pumps?
Intrathecal pumps deliver medication directly to the spinal fluid (learn more). This method provides powerful relief while significantly lowering opioid dosage requirements.
These devices are endorsed by:
When to Consider an Intrathecal Pump
- Oral or IV opioids fail to control pain
- Systemic side effects interfere with quality of life
- Pain affects multiple spinal levels
Benefits of Intrathecal Drug Delivery
Intrathecal pumps can be paired with a handheld Patient Therapy Manager (PTM). This tool enables patients to administer bolus doses during breakthrough pain episodes. Similar to PCA pumps used in hospitals, PTMs enhance independence and satisfaction.
- Pain scores drop by 3–4 points within weeks
- Breakthrough pain episodes decrease significantly
- Sleep, mood, and activity levels improve markedly
- Most patients report increased control and satisfaction

Safety and Side Effects
These devices maintain a strong safety profile. Known complications include:
- Infection (~3%)
- Post-dural puncture headache
- Urinary retention
Most of these issues are manageable using standard medical care.
Cost Considerations
While initial costs can be high, insurance typically covers IDDS for cancer pain. Moreover, the system often becomes cost-effective within 3–8 months, particularly in patients using high-dose or costly opioids.
Ongoing maintenance tends to be more affordable than oral or IV drug regimens.
Limitations
- Long-term outcomes remain under-studied
- Research focuses more on advanced cancer than survivorship
- Further investigation is needed to optimize timing and patient selection
Nevertheless, real-world results continue to validate IDDS as a powerful option for cancer pain relief.
Step Four: Non-Drug and Interventional Support
Complementary therapies address the multifaceted nature of cancer pain:
- Physical therapy – Enhances mobility and strength
- Cognitive-behavioral therapy – Alleviates distress and improves coping
- Spiritual support – Promotes peace and meaning
- Nerve blocks and neurolysis – Disrupt pain signals at the source
- Radiation therapy – Targets tumor-driven pain
Personalized Pain Management Is Key
Each patient experiences pain differently. Therefore, the most effective plan is tailored and includes:
- Continuous reassessment
- Clear communication with care teams
- Willingness to adapt as needed
Cancer Pain Relief Is Within Reach
You don’t have to live in constant pain. With medications, intrathecal pumps, and integrative therapies, lasting cancer pain relief is possible.
At Red Butte Pain Solutions, we work closely with your oncology team to relieve pain and help you reclaim your daily life. Take the next step toward relief in Chandler, Ahwatukee, Laveen, Sun Lakes, Casa Grande, Maricopa, Gilbert, Mesa, Tempe, and South Phoenix.
📞 Call us today at 602-633-4334
🔗 Schedule now

