
Shingles can strike unexpectedly, transforming everyday moments into painful challenges. I recently treated a delightful 82-year-old woman who developed shingles on her right flank. At the time, she was undergoing chemotherapy for cancer, which had weakened her immune system, leaving her vulnerable to viral reactivation. The pain was excruciating—eating, sleeping, and even wearing clothes became unbearable. Her quality of life plummeted, and she needed relief urgently.
Understanding Shingles
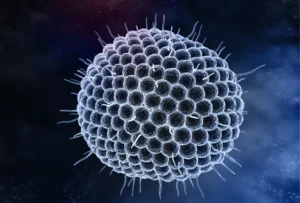
Shingles, or herpes zoster, is caused by the reactivation of the varicella-zoster virus, the same virus responsible for chickenpox. After a person recovers from chickenpox, the virus lies dormant in nerve tissue. Years or decades later, it can reactivate, especially when the immune system is compromised, as it often is with cancer treatments like chemotherapy.
Symptoms of Shingles
- Severe pain: Often the first symptom, even before the rash appears.
- Red rash: Typically on one side of the body or face.
- Blisters: Fluid-filled blisters that eventually crust over.
- Itching and tingling: Affected areas may feel irritated or tingly.
- Sensitivity to touch: Even light contact can cause discomfort.
Our patient experienced sharp pain on her right flank, making even the simplest activities overwhelming. In her case, chemotherapy not only increased her risk for shingles but also made her symptoms more severe.
Risk Factors for Shingles
Several factors increase the risk of developing shingles:
- Age: Risk rises after 50, as immune defenses weaken.
- Weakened immunity: Cancer, chemotherapy, and conditions like HIV increase vulnerability.
- Stress or trauma: Physical or emotional stress may trigger reactivation.
- Medications: Immunosuppressants raise the risk.
- Previous chickenpox: Anyone who’s had chickenpox carries the virus.
Our Treatment Approach
We implemented an aggressive plan to relieve her pain:
- Duloxetine: This nerve pain medication helped balance neurotransmitters, providing significant relief from neuropathic pain.
- Intrathecal steroid injection: Steroids injected into the spinal canal reduced nerve inflammation, offering rapid relief.
This combination of treatments brought her immense relief. She gradually regained the ability to eat, sleep, and wear her favorite clothes—simple joys she had lost. Seeing her smile again after such a difficult time was incredibly rewarding.
Treating Shingles
Effective management involves prompt intervention:
- Antiviral medications: Drugs like acyclovir can reduce severity if started within 72 hours.
- Pain management:
- OTC pain relievers: Acetaminophen or ibuprofen ease mild discomfort.
- Nerve pain medications: Duloxetine, gabapentin, or pregabalin target neuropathic pain.
- Topical treatments: Lidocaine creams help numb affected areas.
- Corticosteroids: These reduce inflammation and may prevent complications.
- Rest and self-care:
- Cool compresses: Apply to soothe the rash.
- Loose clothing: Soft, breathable fabrics reduce irritation.
- Stress reduction: Practice relaxation exercises like deep breathing.
Preventing Shingles
Prevention is especially important for older adults or those undergoing chemotherapy:
- Vaccination:
- Shingrix: Recommended for adults over 50, with over 90% effectiveness.
- Zostavax: An older vaccine, is no longer used and was taken off the market in November 2020.
- Healthy lifestyle:
- Balanced diet and exercise: Support immune function.
- Stress management: Techniques like meditation or yoga reduce stress.
- Avoid spreading the virus:
- Cover the rash: Prevents transmission.
- Hand hygiene: Wash hands frequently.
- Limit contact: Avoid close contact with newborns, pregnant women, or the immunocompromised.
Why Early Treatment Matters
Prompt treatment offers several benefits:
- Reduces pain duration: Shortens acute discomfort.
- Prevents complications: Lowers the risk of postherpetic neuralgia.
- Speeds recovery: Helps patients return to normal activities sooner.
In our patient’s case, her chemotherapy made early intervention even more critical. With the right treatment plan, she was able to find relief and reclaim her quality of life.
Potential Complications of Shingles
Without proper care, shingles can lead to:
- Postherpetic neuralgia: Persistent nerve pain after the rash resolves.
- Vision problems: If shingles affects the eye.
- Neurological issues: Rare cases may involve encephalitis or facial paralysis.
- Skin infections: Open blisters may become infected.
Takeaways from This Case
- Cancer treatment increases risk: Patients undergoing chemotherapy should monitor for shingles symptoms.
- Don’t delay treatment: Early medical attention can prevent complications.
- Comprehensive care works: Combining medications and procedures offers effective relief.
- Consider vaccination: Discuss the shingles vaccine with your doctor if you’re eligible.
Final Thoughts
Shingles is more than just a rash—it’s a painful condition that can severely disrupt daily life, especially for those undergoing cancer treatments. Recognizing symptoms early and understanding risk factors are essential for managing and preventing it.
Our patient’s journey illustrates the importance of addressing shingles promptly, especially in immunocompromised individuals. With the right approach, even severe cases of shingles can be managed, allowing patients to regain comfort and joy.
If You Suspect Shingles
- See a doctor immediately: Early diagnosis is crucial.
- Avoid self-medicating: Seek professional guidance.
- Inform close contacts: Especially those at high risk.
If you have questions about shingles or need guidance, feel free to call us at 602-633-4334 to schedule an appointment or Pre-Register here. We’re here to help you through your health journey. Shingles doesn’t discriminate—if you’ve had chickenpox, you’re at risk. Stay informed, take preventive steps, and seek care promptly if symptoms arise.
